Treatment referral and completion
Treatment referrals are part of interventions that aim to reduce immediate or short-term harms from AOD use, engage and support people affected, and connect people to treatment services where required. As part of care, case management co-ordination involves ongoing treatment planning, goal setting, review and facilitation for the client to achieve their goals, including a supported referral and system navigation support to other services. It includes ensuring links are made with health or social welfare services, and that care is coordinated across care settings and systems (Department of Health 2019).
Key findings
In 2021–22:
- self/family was the most common source of referral (37%)
- three in 4 (76%) episodes ended within 3 months
- around 3 in 5 (58%) treatment episodes had an expected/planned completion
- the median duration of episodes for a clients’ own alcohol or drug use and for someone else’s alcohol or drug use was 5 weeks (35 and 37 days, respectively).
Over the 10-year period to 2021–22:
- source of referral episodes for self/family decreased from 42% in 2012–13 to 37% in 2021–22
- the proportion of episodes with an expected completion decreased from 63% to 58%.
In 2021–22, for all clients:
- the most common source of referral was self/family (37% or 83,607 episodes) followed by health services (32% or 73,383 episodes):
- this referral pattern was consistent for most treatment types
- health services were the most common referral source for withdrawal management (46%), other treatment (41%), information and education (40%) and assessment only (34%) (Table Trt.11).
- diversion referrals fell from 17% to 8% over the same period (Table Trt.11).
- diversion as a referral source was most common for ecstasy (33%) and cannabis (20%) (Table Drg.13).
The most common sources of referral for a client’s own alcohol or drug use and someone else’s alcohol or drug use were similar in 2021–22:
- self/family (37%) was most common for a client’s own alcohol or drug use, followed by health service (32%)
- self/family (36%) was most common for clients receiving treatment for someone else’s alcohol or drug use, followed by health services (30%).
Over the 10-year period to 2021–22, treatment episodes where the referral source was:
- self/family decreased from 42% in 2012–13 to 37% in 2021–22
- health services increased from 24% to 32% over this time (tables Trt.10, Trt.11).
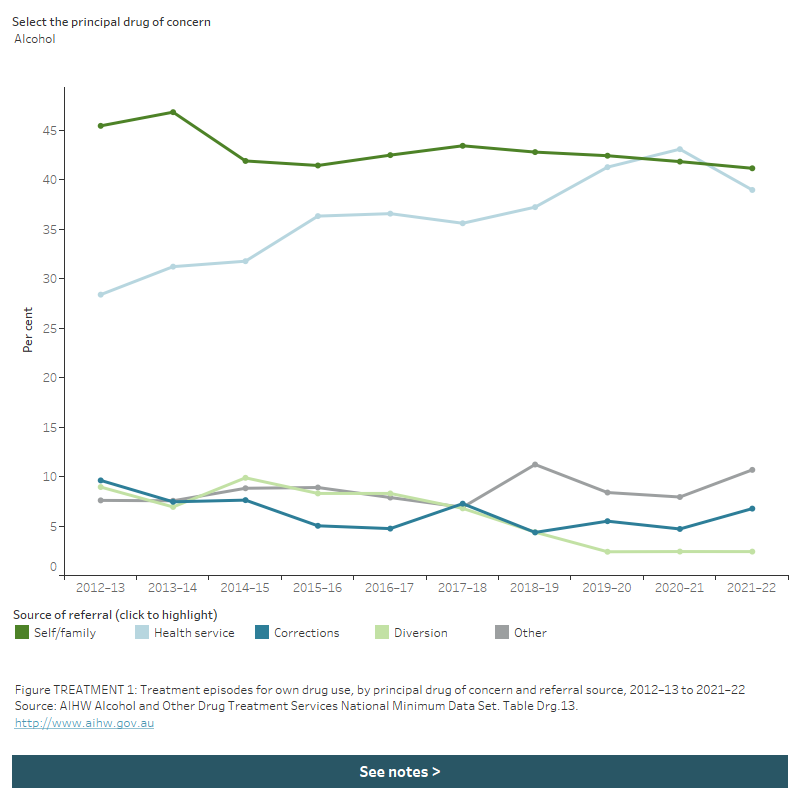
The source of referral varied according to clients’ principal drug of concern. For example, in the 10 years to 2021–22, among episodes for a client’s own alcohol or drug use (Figure TREATMENT 1):
- where alcohol was the principal drug of concern, referrals from health service increased from 28% in 2012–13 to 39% in 2021–22
- where amphetamines were the principal drug of concern, referrals from health service increased from 19% to 26%, while referrals for self/family decreased from 43% to 37%
- where cannabis was the principal drug of concern, the proportion of diversion (police or court diversion program) referrals increased from 2012–13 (32%) to 2014–15 (38%) before falling to 20% in 2021–22
- where a referral came from an ‘other’ referral source, treatment episodes increased from 7.6% in 2012–13 to 16% in 2019–2020, then decreased to 12% in 2021–22.
Figure TREATMENT 1: Treatment episodes for own drug use, by principal drug of concern and referral source, 2012–13 to 2021–22
The line graph shows the proportion of episodes by source of referral among treatment episodes with alcohol as the principal drug of concern. Self/family was the most common source of referral in most years between 2012-13 and 2021-22, accounting for 41.2% of episodes in 2021-22. A filter allows the user to view data for different principal drugs of concern.
Department of Health 2019.National Framework for Alcohol, Tobacco and Other Drug Treatment 2019–29. Canberra: Department of Health. Viewed 23 April 2021.


