Indigenous health and wellbeing
Citation
AIHW
Australian Institute of Health and Welfare (2022) Indigenous health and wellbeing, AIHW, Australian Government, accessed 19 April 2024.
APA
Australian Institute of Health and Welfare. (2022). Indigenous health and wellbeing. Retrieved from https://pp.aihw.gov.au/reports/australias-health/indigenous-health-and-wellbeing
MLA
Indigenous health and wellbeing. Australian Institute of Health and Welfare, 07 July 2022, https://pp.aihw.gov.au/reports/australias-health/indigenous-health-and-wellbeing
Vancouver
Australian Institute of Health and Welfare. Indigenous health and wellbeing [Internet]. Canberra: Australian Institute of Health and Welfare, 2022 [cited 2024 Apr. 19]. Available from: https://pp.aihw.gov.au/reports/australias-health/indigenous-health-and-wellbeing
Harvard
Australian Institute of Health and Welfare (AIHW) 2022, Indigenous health and wellbeing, viewed 19 April 2024, https://pp.aihw.gov.au/reports/australias-health/indigenous-health-and-wellbeing
Get citations as an Endnote file: Endnote

For Aboriginal and Torres Strait Islander people, good health is more than the absence of disease or illness; it is a holistic concept that includes physical, social, emotional, cultural and spiritual wellbeing, for both the individual and the community.
This page highlights some of the key issues in Indigenous health and includes links to more detailed information.
Life expectancy and deaths
Life expectancy and deaths are widely used as indicators of population health. Given current mortality patterns, Indigenous males born in 2015–2017 could expect to live 71.6 years, and Indigenous females 75.6 years (ABS 2018). In general, life expectancy is lower in remote areas, with Indigenous males and females living in Major cities expected to live around 6 years longer than those living in Remote and Very remote areas.
Indigenous death rates have been falling in most age groups over the past 10 years, with the median age at death increasing from 56.5 in 2010 to 61.0 in 2020 (ABS 2021b). In 2020, the leading causes of death among Indigenous Australians were coronary heart disease, diabetes, chronic lower respiratory diseases, cancers of the lung, bronchus and trachea, and intentional self-harm (ABS 2021a).
In the last few years, cancers have overtaken cardiovascular diseases as the most common group of diseases causing deaths among both Indigenous and non-Indigenous Australians. Between 2006 and 2018, the age-standardised death rate for cardiovascular disease among Indigenous Australians fell from 323 to 229 per 100,000, while the cancer death rate rose from 205 to 235 per 100,000 (AIHW 2020).
The Aboriginal and Torres Strait Islander Health Performance Framework provides detailed information on life expectancy and deaths among Indigenous Australians, including infant and child mortality, leading causes of death, avoidable and preventable deaths, and changes over time.
Burden of disease
Conditions that generally cause illness and disability, rather than death, can have a major impact on the health of individuals and communities – for example, depression, arthritis, hearing loss, and asthma. One way of combining the fatal and non-fatal effects of diseases in a comparable way is through burden of disease analysis. This measures the impact of different diseases and injuries in terms of the number of years of healthy life lost due to illness or premature death.
The Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018 found that, in 2018, Indigenous Australians as a whole lost almost 240,000 years of healthy life due to ill-health and premature death – equivalent to 289 years for every 1,000 people. The leading 5 disease groups contributing to burden in Indigenous Australians in 2018 were:
- mental & substance use disorders (such as anxiety, depression, and drug use)
- injuries (such as falls, road traffic injuries, and suicide)
- cardiovascular diseases (such as coronary heart disease and rheumatic heart disease)
- cancer and other neoplasms (such as lung cancer and breast cancer) and
- musculoskeletal conditions (such as back pain & problems and osteoarthritis).
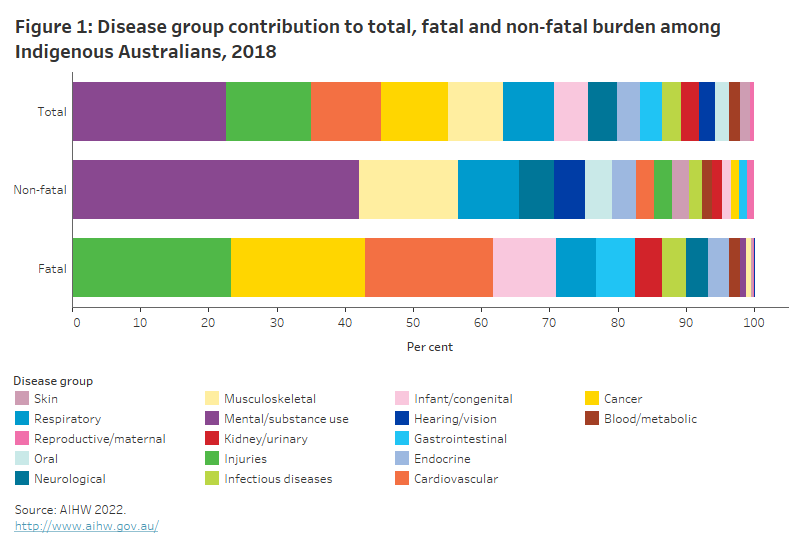
Respiratory diseases also contributed substantially to non-fatal burden, and infant & congenital conditions to fatal burden (Figure 1).
This chart shows the proportion that each of 17 disease groups contributed to total, fatal and non-fatal burden for Indigenous Australians in 2018. Mental & substance use disorders was the greatest contributor to total burden (responsible for 23%) and non-fatal burden (42%). Injuries (including suicide) was the greatest contributor to fatal burden at 23%.
Coronary heart disease (see Glossary) was the leading individual disease contributing to burden among Indigenous Australians in 2018, responsible for 5.8% of total burden. The burden due to coronary heart disease has fallen substantially since 2003, driven by a decrease in fatal burden. Considerable effort has been made to improve cardiac care for Indigenous Australians in recent years through the Better Cardiac Care measures for Aboriginal and Torres Strait Islander people.
Comparison of burden of disease results for Indigenous and non-Indigenous Australians shows that, overall, Indigenous Australians experience burden at 2.3 times the rate of non-Indigenous Australians, but that the absolute gap narrowed between 2003 and 2018.
Social and emotional wellbeing
Social and emotional wellbeing is the foundation of physical and mental health for Indigenous Australians. It is a holistic concept that encompasses the importance of connection to land, culture, spirituality and ancestry, and how these affect the wellbeing of the individual and the community (Gee et al. 2014).
Indigenous Australians’ experience of social and emotional wellbeing varies across different cultural groups as well as across individuals. The concept of social and emotional wellbeing also recognises that a person’s wellbeing is influenced by the social determinants of health, engendered through the inequity of government policies, institutional racism, the effects of colonisation and other past events. See Determinants of health for Indigenous Australians for more information.
Social and emotional wellbeing is not the same as mental health and mental illness, but they can interact and influence each other (PM&C 2017). The National Strategic Framework for Aboriginal and Torres Strait Islander Peoples’ Mental Health and Social and Emotional Wellbeing 2017–2023 recognises this distinction and proposes a model of social and emotional wellbeing with 7 overlapping domains (Gee et al. 2014; PM&C 2017).
For many Indigenous Australians, good mental health is indicated by feeling a sense of belonging, having strong cultural identity, maintaining positive interpersonal relationships, and feeling that life has purpose and value (Dudgeon et al. 2014; Dudgeon & Walker 2015). Conversely, poor mental health can be affected by major stressors such as removal from family, incarceration, death of a close friend or family member, discrimination and unemployment, as well as stressors from everyday life (Gee et al. 2014; PM&C 2017).
In 2018–19, based on self-reported survey responses, an estimated 24% of Indigenous Australians reported having a diagnosed mental health or behavioural condition and 3 in 10 (31%) Indigenous adults reported ‘high or very high’ levels of psychological distress (ABS 2019).
Furthermore, disruptions to family and kinship connections, including inter-generational trauma, have been linked to increased suicide and suicidal behaviour in Indigenous communities (Dudgeon et al. 2021).
For further information on the Framework and social and emotional wellbeing, see the Indigenous Mental Health & Suicide Prevention Clearinghouse.
Suicide and self-harm
Reducing deaths by suicide and suicidal behaviour among Indigenous Australians is an issue of major concern for many Indigenous communities and a public health priority for all Australian governments. Data from 2016–2020 show that the rate for suicide of Indigenous Australians is almost twice the rate of non-Indigenous Australians, with the differences being greater for people aged under 45 (AIHW 2021a). Suicide was the fifth leading cause of death among Indigenous Australians in 2020, accounting for 5.5% of all deaths, and the 14th leading cause of death for all Australians (1.9% of all deaths). It was also the leading cause of death for Indigenous children aged 5–17 (ABS 2021a).
Suicide and self-harm behaviours arise from a complex web of personal, social and historical factors (Dudgeon et al. 2017), but they can be prevented. More about suicide prevention among Aboriginal and Torres Strait Islander people can be found on the Indigenous Mental Health and Suicide Prevention Clearinghouse.
Hearing health, eye health and oral health
Oral and hearing health problems are two issues that particularly affect Indigenous children, especially those living in remote areas.
Otitis media (inflammation and/or infection of the middle ear) is the main condition contributing towards hearing loss in Indigenous children. Experiencing hearing loss in childhood can affect speech and language development, and may lead to behavioural problems, early school leaving, limited employment options and increased contact with the criminal justice system (Burns & Thomson 2013).
Indigenous children are more likely than non-Indigenous children to experience tooth decay and to be hospitalised for dental problems (AIHW 2020). Several factors contribute to the poorer oral health of Indigenous children, including social disadvantage and lack of access to appropriate diet and dental services.
Specific programs such as the Northern Territory Remote Aboriginal Investment Oral Health Program, the Northern Territory hearing health outreach program, and the Queensland Deadly Ears program aim to diagnose and treat these problems and reduce their impact on the Indigenous community.
Vision loss has a profound impact on a person’s quality of life and ability to perform everyday activities, for example, by limiting opportunities for physical mobility, work, education and social engagement (Razavi et al. 2018). Preventable vision problems, such as trachoma, diabetic retinopathy and cataracts (see Glossary), affect Indigenous Australians aged 40 and over at much higher rates than non-Indigenous Australians of the same age. The Indigenous eye health measures annual report provides an evidence base for monitoring changes in Indigenous eye health, identifying inequalities and highlighting potential gaps in service provision.
It’s not the same for everyone everywhere
On average, Indigenous Australians living in remote areas having higher rates of disease burden and lower life expectancy compared with those in non-remote areas. Key contributors to this include differences in educational and employment opportunities, in access to health services, in housing circumstances, and in other factors that support healthy behaviours (such as the availability and cost of fresh fruit and vegetables). But areas of relative advantage and disadvantage also exist within these regions. Local areas and communities may experience different issues and outcomes to others and have different needs and priorities. Looking at variations across smaller geographic areas can help to highlight specific areas of need, so that programs and services can be directed where they will be of most benefit.
Local insights for local needs
The Regional Insights for Indigenous Communities (RIFIC) website brings together a range of regional statistics about the health and wellbeing of Aboriginal and Torres Strait Islander people and communities. It aims to help communities set priorities and participate in joint planning with governments and service providers.
The Stolen Generations and their families are a particular group of Aboriginal and Torres Strait Islander people who experience greater disadvantage than other Indigenous Australians. Analysis of data from the 2014–15 National Aboriginal and Torres Strait Islander Social Survey showed that people who reported being removed from family were more likely than those who did not to have been imprisoned or arrested in the previous 5 years, to have low income, to have poor self-assessed health, to have poor mental health, and to have experienced homelessness in the previous 10 years. This disadvantage persisted through the generations, with adult descendants and co-resident children also experiencing poorer health and wellbeing outcomes compared to other Indigenous Australians (AIHW 2019a, 2019b).
The Stolen Generations
Between approximately 1910 and 1972, thousands of Indigenous children were forcibly removed from their families and communities as a part of government policies across Australian jurisdictions. The Bringing them Home report (HREOC 1997) estimated that this practice affected between 1 in 10 and 1 in 3 Indigenous children during that period.
In 2018–19, there were an estimated 33,600 Stolen Generations survivors across Australia. Around 1 in 3 Indigenous Australian adults were estimated to be descendants of the Stolen Generations (AIHW 2021a).
What about the burden due to COVID-19?
The analyses done for the most recent burden of disease study produced estimates for the year 2018, and therefore did not include COVID-19.
For more information on the impact of COVID-19 on Aboriginal and Torres Strait Islander people, see 'Chapter 1 The impact of a new disease: COVID-19 from 2020, 2021 and into 2022’ and 'Chapter 3 Changes in Aboriginal and Torres Strait Islander people's use of health services in the early part of the COVID-19 pandemic' in Australia’s health 2022: data insights.
Where do I go for more information?
For more information on Indigenous health and wellbeing, see:
- Aboriginal and Torres Strait Islander Health Performance Framework
- Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018
- Indigenous Mental Health & Suicide Prevention Clearinghouse
- Department of Health Aboriginal and Torres Strait Islander health
Visit Indigenous Australians for more on this topic.
References
ABS (Australian Bureau of Statistics) (2018) Life tables for Aboriginal and Torres Strait Islander Australians, 2015–2017, ABS website, accessed 8 March 2022.
ABS (2019) National Aboriginal and Torres Strait Islander Health Survey, 2018–19, ABS website, accessed 20 March 2022.
ABS (2021a) Causes of death, Australia, 2020, ABS website, accessed 20 March 2022.
ABS (2021b) Deaths, Australia, 2020, ABS website, accessed 8 March 2022.
AIHW (Australian Institute of Health and Welfare) (2019a) Aboriginal and Torres Strait Islander Stolen Generations and descendants: numbers, demographic characteristics and selected outcomes, AIHW, Australian Government, accessed 8 March 2022.
AIHW (2019b) Children living in households with members of the Stolen Generations, AIHW, Australian Government, accessed 8 March 2022.
AIHW (2020) Aboriginal and Torres Strait Islander Health Performance Framework, AIHW, Australian Government, accessed 8 March 2022.
AIHW (2021a) Aboriginal and Torres Strait Islander Stolen Generations aged 50 and over: updated analyses for 2018–19, AIHW, Australian Government, accessed 22 March 2022.
AIHW (2021b) Deaths by suicide amongst Indigenous Australians, AIHW website, accessed 22 March 2022.
AIHW (2022) Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018, AIHW, Australian Government, accessed 22 March 2022.
Burns J and Thomson N (2013) ‘Review of ear health and hearing among Indigenous Australians’, Australian Indigenous Health Bulletin, 13(4):1–22.
Dudgeon P, Blustein S, Bray A, Calma T, McPhee R and Ring I (2021) Connection between family, kinship and social and emotional wellbeing. Produced for the Indigenous Mental Health and Suicide Prevention Clearinghouse, AIHW, Australian Government, Canberra.
Dudgeon P, Calma T and Holland C (2017) ‘The context and causes of the suicide of Indigenous people in Australia’, Journal of Indigenous Wellbeing, 2(2):5–15.
Dudgeon P, Cox A, Walker R, Scrine C, Kelly K, Blurton D, Bolardaras J, Brackness C, Brennan T, Butorac A, Charles A, Collard L, Duffin W, Grogan G, Hams K, Hansen C, Holland C, Ingram D, Mascall C, Mia T, Miller D, Mcguire V, Murray B, Mcgrady G, Peckham M, Riley B, Ryder A, Swift S and Taylor N (2014) Voices of the peoples: The national empowerment project research report 2015, Perth: National Empowerment Project, University of Western Australia.
Dudgeon P and Walker R (2015) ‘Decolonising psychology: discourses, strategies and practice’, Journal of Social and Political Psychology, 3(1):276–297.
Gee G, Dudgeon P, Schultz C, Hart A and Kelly K (2014) ‘Social and emotional wellbeing and mental health: an Aboriginal perspective’, in Dudgeon P, Milroy H and Walker R (eds) Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice (2nd edn), Department of the Prime Minister and Cabinet, Australian Government, Canberra.
HREOC (Human Rights and Equal Opportunity Commission) (1997) Bringing them home, Spinney, Sydney.
PM&C (Department of the Prime Minister and Cabinet) (2017) National Strategic Framework for Aboriginal and Torres Strait Islander peoples’ mental health and social and emotional wellbeing 2017–2023, PM&C, Australian Government, accessed 9 March 2022.
Razavi H, Burrow S and Trzesinski A (2018) ‘Review of eye health among Aboriginal and Torres Strait Islander people’, Australian Indigenous Health Bulletin, 18(4), accessed 29 March 2022.


