What is health?
Citation
AIHW
Australian Institute of Health and Welfare (2022) What is health?, AIHW, Australian Government, accessed 16 April 2024.
APA
Australian Institute of Health and Welfare. (2022). What is health?. Retrieved from https://pp.aihw.gov.au/reports/australias-health/what-is-health
MLA
What is health?. Australian Institute of Health and Welfare, 07 July 2022, https://pp.aihw.gov.au/reports/australias-health/what-is-health
Vancouver
Australian Institute of Health and Welfare. What is health? [Internet]. Canberra: Australian Institute of Health and Welfare, 2022 [cited 2024 Apr. 16]. Available from: https://pp.aihw.gov.au/reports/australias-health/what-is-health
Harvard
Australian Institute of Health and Welfare (AIHW) 2022, What is health?, viewed 16 April 2024, https://pp.aihw.gov.au/reports/australias-health/what-is-health
Get citations as an Endnote file: Endnote

On this page:
Health can be viewed as the presence or absence of disease or medically measured risk factors in an individual. However, more broadly, health is 'a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity' (WHO 1946). Health reflects the complex interactions of a person's genetics, lifestyle, and environment.
Australians have good health, in general, and access to an effective health system. How do we know this? We compare Australia with other Organisation for Economic Co-operation and Development (OECD) countries and we use the Australian Health Performance Framework to assess the health of our population and health system. The Framework outlines health indicators that describe specific elements of our health or aspects of our health system's performance. It also compares data for different population groups, different geographic regions, and internationally. The Framework includes the domains of health status, determinants of health, and the health system (see also the Health system domain in Australia's health topic summaries).
What influences health?
There is a close relationship between people's health and the circumstances in which they grow, live, work, play and age (Commission on Social Determinants of Health 2008). Factors such as income, employment, education, housing, social connections and support, the environment, behaviours, and genetics influence health.
These many factors, known as 'health determinants', may be risk or protective factors, and interact to influence the health of individuals and communities.
The framework in Figure 1 depicts risk factors from 'downstream' behavioural and biomedical factors to 'upstream' risk factors (further away in the causal chain from the health outcome), which include broad features of society such as the natural and built environment, culture and affluence. The factors within each box in Figure 1 can interact and are closely related to each other, and all play a large role in determining health and health outcomes.
The socioeconomic characteristics in the framework – including education; employment; income; family circumstances and early childhood; housing; working conditions; and social support – have each been shown to affect health outcomes, with overlap between them: for example, people with higher education are more likely to earn higher incomes. They have an important influence on health inequities – the avoidable differences in health status seen within and between groups and countries (Commission on Social Determinants of Health 2008).
See Social determinants of health.
Figure 1: Framework for determinants of health
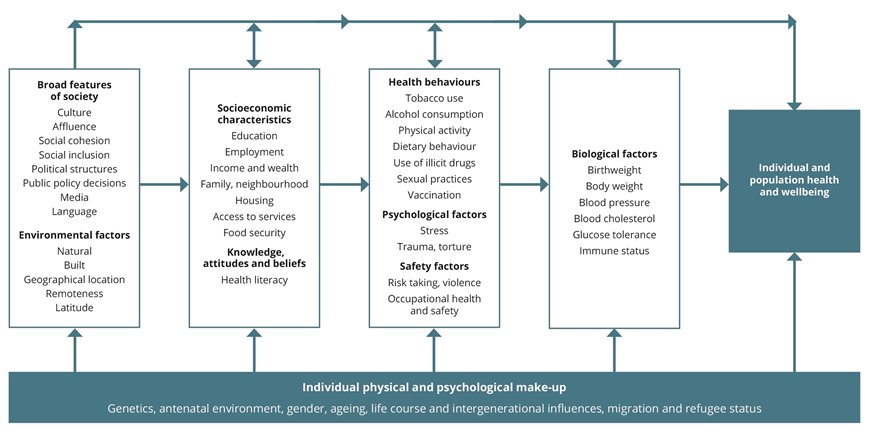
Even more broadly, commercial environments (for example, advertising and supply chains) and digital environments (for example, digital technology and resources such as electronic medical records and advances to diagnostic and therapeutic tools) can be determinants of health; see also the National Preventive Health Strategy 2021–2030 (Department of Health 2021a).
See the Determinants of health domain in Australia's health topic summaries for more information.
Measuring health
Many measures can be used to describe the health of an individual or a population. Some commonly used measures are listed in Table 1.
| Measure | Description |
|---|---|
| Life expectancy | The number of years of life, on average, remaining for an individual at a particular age if death rates do not change. The most commonly used measure is life expectancy at birth. |
| Mortality | The number of deaths in a population in a given period. |
| Morbidity | Ill health in an individual and levels of ill health within a population (often expressed through incidence, prevalence and comorbidity measures – see Glossary). |
| Disability-adjusted life year (DALY) | One year of healthy life lost due to illness and/or death. DALYs are calculated as the sum of the years of life lost due to premature death and the years lived with disability due to disease or injury. |
| Health-adjusted life expectancy | The average length of time an individual at a specific age can expect to live in full health; that is, time lived without the health consequences of disease or injury. |
| Self-assessed health status | An individual's own opinion about how they feel about their health, their state of mind and their life in general. |
These measures are useful to observe trends over time, compare different population groups and geographic regions, and monitor certain health conditions. Health measures enable differences in health outcomes to be identified. These measures are discussed in more detail in the Health status and Health of population groups domains in Australia's health topic summaries.
Health system interventions
The health system supports the health of the nation by treating illness, preventing disease, and maintaining people's health. Health system overview describes how Australia's health system works. A functioning health system ensures that people remain as healthy as possible and for as long as possible. Australia's health system facilitates this by providing services such as hospital care and primary health care (such as general practice and allied health services) and access to preventative measures such as immunisation and vaccination. Health promotion and health protection is also a crucial part of the system which supports people's health. See also the Health system domain in Australia's health topic summaries.
Australian Charter of Healthcare Rights
The Australian Charter of Healthcare Rights (2nd edition) (ACSQHC 2020) describes the 7 key rights of patients and consumers who seek or receive health care:
- Access – the right to access health care services and treatment that meet their needs
- Safety – the right to safe and high-quality health care that meets national standards in a safe environment
- Respect – the right to be treated as an individual, with dignity and respect, and to have culture, identity, beliefs, and choices recognised and respected
- Partnership – the right to be involved in open and honest communication, to make decisions with health care providers, and to choose who to include in planning and decision making
- Information – the right to clear information about conditions and services, to assistance when needed to understand health information, and to access personal health information
- Privacy – the right to privacy and confidentiality of personal information
- Give feedback – the right to comment on care, to have concerns dealt with transparently and in a timely manner, and to share experiences and participate to improve quality of care and health services (ACSQHC 2020).
The application of the Charter to the health system is informed by 3 guiding principles:
- the right of everyone to access health care
- the commitment of the Australian Government to international agreements recognising the right to health
- the acknowledgement of and respect for the different cultures and ways of life in Australian society.
Health data in Australia
The availability of quality, timely, accessible and comprehensive health data is important for measuring health status and service use, and considering improvements to support the health and wellbeing of Australians.
Despite recent information improvements and enhancements and the fact that Australians have access to high quality information in many areas of health, there are aspects of health and the health system that we don't have adequate information on. Data gaps exist where there are no national data currently available or where data collected are not comprehensive or in a format that can be analysed or used meaningfully.
These gaps in available information can limit the capacity for population health monitoring, research, planning and policy development in important areas of the health system. Some gaps in Australian health data include:
- a lack of person-centred data. Some data are event rather than person based and it is not always possible to see how one person uses multiple services.
- data on primary health care activity and outcomes (the available health data – drawn from Medicare – provide a wide and comprehensive coverage of health care use. However, as with any data source, there are still gaps. For example, Medicare does not contain information about why some healthcare services are used and others are not, as well as diagnostic and health outcome information)
- information on some population groups – such as culturally and linguistically diverse populations and refugees.
Data integration
Data integration (a process combining information from multiple sources, while preserving privacy) is increasingly being used to fill knowledge and data gaps across the health information system. Demand continues to grow both for one-off data integration and more enduring integrated data assets to answer complex cross-sector and cross-jurisdictional health questions. For example, the Analysis of cancer outcomes and screening behaviour for national cancer screening programs in Australia combined data from the National Bowel Cancer Screening Program, BreastScreen Australia, and the National Cervical Screening Program. It was found that screen-detected cancers were less likely to cause death than non-screen-detected cancers (AIHW 2018). In addition, a number of Multi-source Enduring Linked Data Assets have emerged in Australia, including the National Integrated Health Services Information Analysis Asset and the Multi-Agency Data Integration Project.
Health data and COVID‑19
Timely and accurate health data from a range of sources have been pivotal in informing responses to the COVID‑19 pandemic. The pandemic has made the value of health data, as well as the gaps and issues in the collection and use of that data, more prominent and visible, while also enabling some data sharing and timely improvements.
For more information, see 'Chapter 10 Health information in Australia: an evolving landscape with an integrated future' in Australia's health 2022: data insights.
The impact of COVID‑19
The COVID-19 pandemic has affected the health and wellbeing of Australians. The pandemic has had direct health effects – for example for those who contracted the disease – and a multitude of indirect health impacts. These indirect impacts have stemmed from the many measures implemented to reduce the spread of the virus and support our health system, such as lockdowns and stay-at-home orders.
These measures have also had the potential to impact people's mental and emotional wellbeing, health care for other conditions, and health behaviours. In addition, they have had a broader impact on other factors important to health, such as employment, income, family functioning, and social connectedness. However, there have also been improvements in other aspects of health, such as reductions in injuries (including fewer road deaths) and fewer cases of other infectious diseases such as influenza in 2020 (AIHW 2021c).
For more information see Social isolation and loneliness, Employment and unemployment, and 'Chapter 1 – The impact of a new disease: COVID‑19 from 2020, 2021 and into 2022' and 'Chapter 2 – Changes in the health of Australians during the COVID‑19 period' in Australia's health 2022: data insights.
The measures designed to control the spread of the virus have also had notable impacts on the healthcare system and the way people engage with healthcare services, including:
- reductions in the assessment and screening rates for some medical conditions, such as breast cancer screening (AIHW 2020a)
- increased demands on hospital intensive care units (AIHW 2020b)
- postponement of many non-essential surgical procedures (AIHW 2021a)
- inclusion of more telehealth items in the Medicare Benefits Schedule (MBS), increasing the breadth and accessibility of healthcare services (AIHW 2021b; Department of Health 2021b).
Where do I go for more information?
For more information on health definitions see:
- World Health Organizatio, (WHO)
- Department of Health National Preventive Health Strategy 2021–2030.
ACSQHC (Australian Commission on Safety and Quality in Health Care) (2020) Australian charter of healthcare rights (2nd edition), ACSQHC website, accessed 23 February 2022.
AIHW (Australian Institute of Health and Welfare) (2018) Analysis of cancer outcomes and screening behaviour for national cancer screening programs in Australia, AIHW, Australian Government, accessed 23 February 2022.
AIHW (2020a) Cancer screening and COVID-19 in Australia, AIHW, Australian Government, accessed 23 February 2022.
AIHW (2020b) Emergency department care activity, AIHW, Australian Government, accessed 23 February 2022.
AIHW (2021a) Elective surgery, AIHW, Australian Government, accessed 23 February 2022.
AIHW (2021b) Impacts of COVID‑19 on Medicare Benefits Scheme and Pharmaceutical Benefits Scheme: quarterly data, AIHW, Australian Government, accessed 23 February 2022.
AIHW (2021c) The first year of COVID‑19 in Australia: direct and indirect health effects, AIHW, Australian Government, accessed 23 February 2022.
Commission on Social Determinants of Health (2008) Closing the gap in a generation: health equity through action on the social determinants of health – Final report of the commission on social determinants of health, WHO, accessed 11 March 2022.
Department of Health (2021a) National preventive health strategy 2021–2030, Department of Health, Australian Government, accessed 11 March 2022.
Department of Health (2021b) Ongoing MBS telehealth services, Department of Health website, accessed 23 February 2022.
WHO (1946) Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19–22 June, 1946, WHO, New York, accessed 23 February 2022.


