Summary
Chronic Disease Management (CDM) services are Medicare-subsidised services provided by General Practitioners (GPs) and are available to people with chronic or terminal medical conditions. Rather than a having a list of eligible conditions, a GP can determine whether a patient would benefit from a structured approach to care, based on their clinical judgement and accounting for the eligibility criteria and guidance contained within the Medicare Benefits Schedule (MBS) (Department of Health 2014).
The CDM services cover the coordination, creation and review of several care planning tools:
A General Practitioner Management Plan (GPMP), which is a plan of action agreed between a patient and their GP. The plan identifies the patient’s health and care needs, sets out the services to be provided by the GP, and lists the actions the patient can take to help manage their condition.
Team Care Arrangements (TCAs), for patients with complex care needs requiring multidisciplinary care, which provide Medicare-subsidised care (5 services per calendar year) from selected allied health care providers for individual treatment services where the patient also has a GPMP.
Multidisciplinary Care Plans, are written plans that are prepared for a patient by a health or care provider often for patients in a Residential Aged Care Facility and describe the treatment and services to be provided to the patient by the collaborating providers.
It is recommended that GPMPs, TCAs and multidisciplinary care plans be regularly reviewed by the GP and the patient. Figure 1 shows patient pathways for CDM services.
Figure 1: Patient pathways to the CDM and Medicare-subsidised allied health services
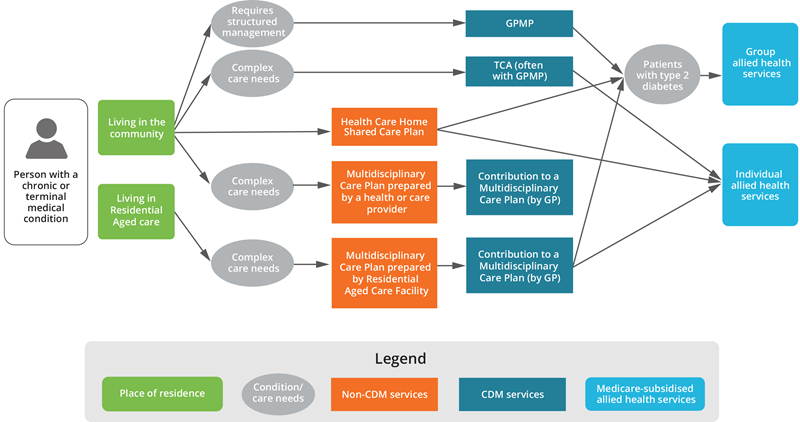
Note: The Healthcare Homes trial began in October 2017 and ended on 30 June 2021. This pathway was available to patients in 2019, which is the analysis period for the bulk of this report.
This web report explores the use of CDM services and Medicare-subsidised allied health services in 2019. More than 3.8 million Australian’s had a CDM service in 2019, with GPMPs and TCAs being the most used services (see Table 1). The use of GPMPs and TCAs was highest among patients aged 75–84 and varied according to remoteness and socioeconomic area (see Profile of CDM patients). The use of GPMP and TCA services has increased steadily over the last decade, with close to $1 billion paid by Medicare for CDM services in 2019 (see Trends in GPMP and TCA item use and Spending on CDM services).
In 2019, over 2.4 million patients claimed around 8.2 million Medicare-subsidised individual allied health services, with the most used services being podiatry, physiotherapy, and dietetics (see Table 4a). The use of Medicare-subsidised individual allied health services has increased steadily over the past decade (see Trends in allied health service use). Medicare paid $446 million in benefits for these services, with bulk billing rates varying considerably between the services (see Spending on allied health services). Of patients who accessed Medicare-subsidised individual allied health services in 2019, 37% used all 5 services. The number of services used decreased with increasing remoteness (See Patterns of allied health service use).
COVID-19 impact
The COVID-19 pandemic changed the way that many Australians’ accessed health care. For CDM and Medicare-subsidised allied health services, a series of telehealth services were introduced to enable care to continue to be delivered. Telephone rather than videoconference was used for most CDM telehealth services in 2020. Telephone CDM services peaked in May, decreased in June/ July and rose again in August before continuing to decrease to December 2020 (See Impact of COVID-19 on CDM and Medicare-subsidised allied health services).
References
Department of Health (2014) Questions and Answers on the Chronic Disease Management (CDM) items, Department of Health website, accessed 24 March 2021.


