How did patterns of dementia deaths vary during the pandemic when other health conditons were recorded?
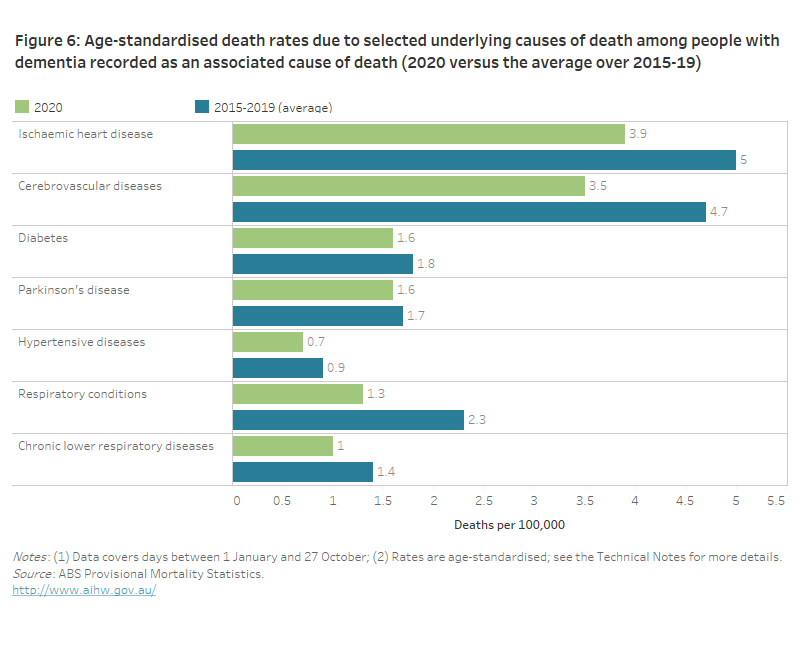
Measures in response to the pandemic likely led to reduced mortality among people with a wide range of other medical conditions. Figure 6 shows age-standardised death rates for 7 selected underlying causes of death recorded among people who had dementia recorded as an associated cause of death. The selected underlying causes include conditions frequently reported on death certificates among people who also have dementia recorded, as well as respiratory conditions, which COVID-19 may have caused or exacerbated. Respiratory conditions encompass acute conditions (like pneumonia and influenza) and chronic conditions (like asthma and emphysema).
During the first 10 months of 2020, the age-standardised death rates for all the selected causes were lower than the average rate during the same months in previous years (2015–19); it is notable that even though COVID-19 often causes or exacerbates respiratory conditions among people who die due to the virus, the overall rate of respiratory conditions was still lower during the pandemic period (see Figure 6).
While lower rates of deaths from ischaemic heart disease and cerebrovascular diseases have links to the public health measures put in place during 2020 as a response to the pandemic, they largely reflect the steadily declining mortality from these conditions since the late 1960s (AIHW 2012; ABS 2020a). See Figure 2 for mortality trends by these conditions over the last 5 years.
Figure 6: Age-standardised death rates due to selected underlying causes of death among people with dementia recorded as an associated cause of death (2020 versus the average over 2015-19).
This bar graph shows age standardised death rates summed over 1 January to 27 October, for deaths due to selected underlying causes of death among people who died with dementia. It compares rates in 2020 to the average rates for the period 2015 to 2019, and shows that the 2020 rates for all the selected causes were lower than the average rates over 2015-19, including for respiratory conditions.
Pneumonia and influenza were less common among people who died with dementia during the pandemic than in previous years
Older people, including those with dementia, are highly vulnerable to suffering complications and dying from transmissible respiratory infections. For example, in 2019, the median age of people who died due to influenza and pneumonia was 89 years (ABS 2020e). Intricate rules for certifying deaths can influence whether pneumonia and influenza are recorded as an underlying or an associated cause of death, so incorporating all causes of death provides a more complete picture of how these conditions influence deaths among people who die with dementia recorded on their death certificates. Together, they can also provide an indication of the effect that efforts to suppress the spread of COVID-19 have had on the spread of other transmissible infections among people with dementia.
Although some years experience significantly worse outbreaks of respiratory infections than others, there has been a clear seasonal peak in the number of infections due to influenza and pneumonia in recent years (FluTracking Australia 2020). The number of deaths from these conditions among people with dementia recorded on their death certificate also shows a clear seasonal trend in recent years. Although it is not possible to present age-standardised rates due to low numbers, Figure 7 shows the number of deaths over 4-week periods among people who had dementia as well as influenza or pneumonia, recorded on their death certificate:
- the number of deaths due to influenza or pneumonia among people with dementia in 2020 remained very low across the entire 10-month period, peaking at 4 deaths in late February/March (13 deaths in total). In contrast, over 2015–19, the average number of deaths increased from 4 deaths in late March/April to 49 deaths in August/early September (an average of 187 deaths in total)
- the number of deaths among people who died due to dementia and with influenza or pneumonia in 2020 did not show the usual seasonal increase during the winter months—168 people died in late March/April and 123 people died in August/early September (1,390 deaths in total). In contrast over 2015–19, the average number of deaths increased from 167 in late March/April, to 243 in August/early September (an average of 2,053 deaths in total).
These data support the findings of other studies that infection control measures introduced in Australia in response to the pandemic, Australians’ adherence to these measures, and the increased uptake in influenza vaccinations has reduced the spread of other transmissible infections and their subsequent mortality, including among people living with dementia (Department of Health 2020; ABS 2020a; ABS 2021).
Figure 7: Influenza or pneumonia among people with dementia recorded on their death certificates (2020 versus average of 2015-19).
This figure includes two line graphs that show the number of influenza and pneumonia deaths among people with dementia, over 4-week periods from 1 January to 27 October 2020, and the corresponding 4 week averages over the period 2015 to 2019. The first graph shows the number of deaths due to influenza or pneumonia when dementia was an associated cause of death. The second graph shows the number of deaths due to dementia when influenza or pneumonia were associated causes of deaths. Both graphs show that there were fewer influenza or pneumonia deaths in 2020 compared to 2015-19.


