Methods
Scope
There were 23,445 patients in the cohort analysed in this project. These were patients who were:
- first admitted to a public hospital with a diagnosis of intracranial injury in a participating jurisdiction from 1 July 2013 to 30 June 2015; and
- aged 0 to 64 years; and
- had a mode of admission that was not Admitted patient transferred from another hospital.
In-scope hospital admissions are referred to in this publication as ‘initial TBI hospitalisations’ or ‘initial TBI admissions’. Initial TBI hospitalisations were not preceded by any other TBI hospital admission between 1 July 2010 and 30 June 2013. Some patients may have had a hospital admission for TBI before 1 July 2010, but it was not possible to detect this in the data source.
An initial TBI hospitalisation is the initial admission and all related contiguous (or adjoining) admissions. For example, a record for the same person with a subsequent admission date on the same day as the initial separation date was assumed to be a ‘contiguous episode’. This covers cases were a patient might have been transferred from one hospital to another or a change in care type within the same hospital (for example, from acute to sub-acute).
Reference period
The report explores patient pathways and service utilisation for the following time periods:
- during the initial TBI hospitalisation (between 1 July 2013 and 30 June 2015)
- two years before the initial TBI hospitalisation (covering the period 1 July 2011 to 30 June 2013) and
- two years after the initial TBI hospitalisation (covering the period 1 July 2015 to 30 June 2017).
Further explanation of scope
This study includes patients with either a principal diagnosis or an additional diagnosis of Intracranial injury (S06 in the ICD-10-AM) (see Table 2). A principal diagnosis is the condition chiefly responsible for hospitalisation; an additional diagnosis is a condition that coexists with a principal diagnosis or a condition that arose during hospitalisation.
Diagnosis codes were recorded using the ICD-10-AM 8th edition. Procedures were reported using the Australian Classification of Health Interventions (ACHI) 8th edition.
The time frame for the first TBI hospitalisation was chosen based on the need for:
- several years of data both before and after the first TBI hospitalisation for comparison purposes and
- the need for a large enough cohort to enable robust data analysis.
Not all jurisdictions participated in NIHSI AA v0.5. Participating jurisdictions were New South Wales, Victoria, South Australia and Tasmania (66% of the Australian population). Non-participating jurisdictions were Queensland, Western Australia, the Northern Territory and the Australian Capital Territory.
The age of patients in the cohort was restricted to persons aged under 65 to avoid including confounding data that may have been the result of age-related degenerative brain disorders such as dementia.
Patients who had a mode of admission that was Admitted patient transferred from another hospital were excluded to avoid double-counting these patients.
A minority of TBI hospitalisations from 1 July 2013 to 30 June 2015 were at private hospitals. These hospitalisations are excluded from this analysis because private hospital participation in the NIHSI AA v0.5 is very limited and data linkage quality is poor.
Data source
Data are from the National Integrated Health Services Information Analysis Asset (NIHSI AA) (version 0.5), that links data on admitted patient care (hospitalisations), emergency department presentations, non-admitted patient care, deaths, prescription medications, Medicare services and residential aged care (RAC). See Table 1 for the components that were used in this project.
By enabling the matching of records that are highly likely to pertain to the same person, NIHSI AA data allows analysis of service use and provision across specific parts of the health care system and across time.
The NIHSI AA (v0.5), contains 7 years of de-identified data from 2010–11 to 2016–17. Data from 2010–11 are not used in this project as it is outside the 6-year reference period.
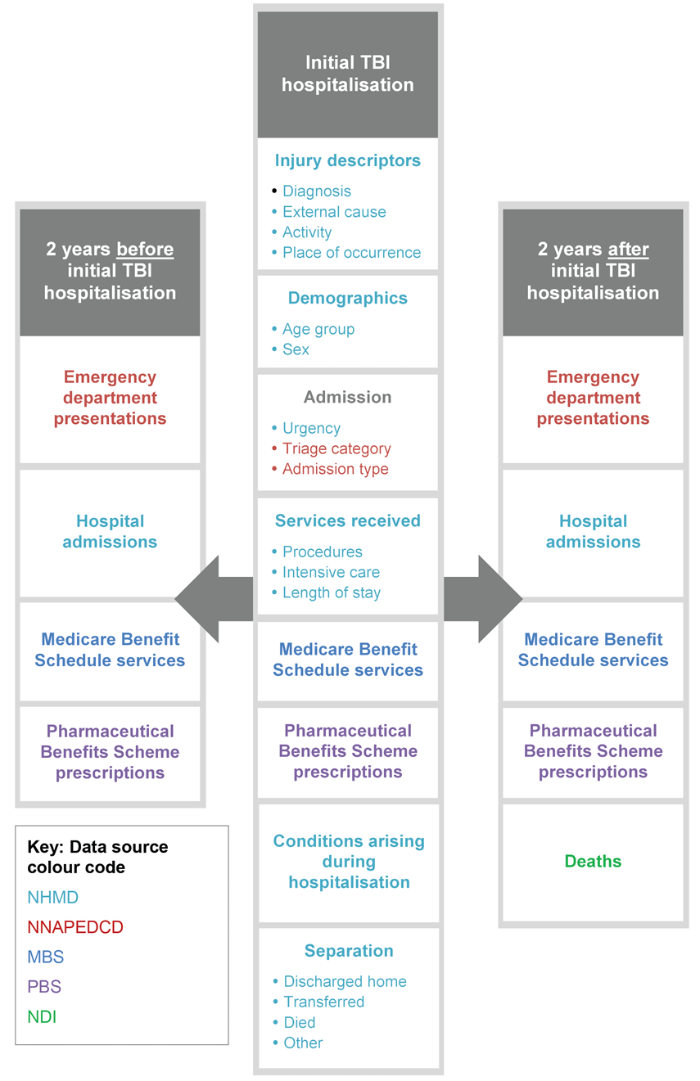
Diagrammatic overview
Figure 1 shows the information analysed in the project and the temporal scope of the project.
| Source data set | Type of information |
|---|---|
| AIHW National Hospital Mobidity Database (NHMD) | Admitted patient care services (in all public and, where available, private hospitals) |
| AIHW National Non-Admitted Patient Emergency Department Care Database (NNAPEDCD) | Emergency department (ED) services |
| Department of Health Medicare Benefits Schedule (MBS) | Clinically relevant services rendered by an appropriate health practitioner listed on the MBS |
| Department of Health Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Benefits Scheme (RPBS) | Pharmaceuticals prescribed that are partially or fully funded by the Australian Government |
| National Deaths Index (NDI) | Deaths |


