Prescribing in primary care
This section presents data for the prescribing in primary care indicators supplied by Australia to the HCQO collection. It compares these data with the HCQO results for other OECD countries, and comments on the comparability of the data provided to the OECD specification (OECD 2021).
Medicines can contribute to quality of life by curing or relieving the symptoms of illness. They can also prevent complications in existing health conditions or delay the onset of disease. However, the overuse, underuse, or misuse of prescription medicines may lead to health hazards and wasteful expenditure (OECD 2021).
The OECD published all prescribing in primary care indicators in OECD.Stat and a selection of prescribing in primary care indicators in Health at a Glance 2021. Australia submitted data for all 11 prescribing in primary care indicators:
- People with diabetes with at least one prescription of cholesterol lowering medication
- People with diabetes with prescription of first choice antihypertensive medication
- Older adults with prescription of long-term benzodiazepines or related drugs
- Older adults with prescription of long-acting benzodiazepines or related drugs
- Proportion of older adults prescribed antipsychotics
- Patients with long-term prescription of any anticoagulating drug in combination with an oral nonsteroidal anti-inflammatory drug (NSAID)
- Total volume of antibiotics for systemic use
- Volume of second line antibiotics as a share of total volume
- Polypharmacy among people aged 75 and over
- Overall volume of opioids prescribed
- Proportion of the population who are chronic opioid users.
The indicator definitions can be viewed here: Prescribing indicator definitions
Overall data comparability and methods
The most recent data supplied by Australia for the prescribing in primary care indicators were for 2020. Data from other OECD countries published on OECD.Stat for 2020 are used for comparison and calculation of OECD averages in this section. These data were extracted from the OECD.Stat database in November 2021, and may not reflect subsequent updates made to the database.
The denominators used in the calculation of the indicators comprise the population in the national prescribing database, rather than the total population estimates (OECD 2021). For Australia, this was calculated as a count of people who were dispensed medicines covered under PBS arrangements in the relevant year. The indicators are presented on the same basis here.
Health at a glance 2021 notes that differences in data sources and coverage may affect calculation of prescription rates (OECD 2021). For example, the PBS data collection contains information on all prescription medicines that qualify for a benefit under the National Health Act 1953 and for which a claim has been processed. Hence, the Australian data include prescriptions dispensed at community pharmacies, private hospital pharmacies, and prescriptions provided to public hospital outpatients and admitted day patients. Meanwhile, data for Austria, Latvia, Estonia, Portugal, Spain, and Sweden include data for primary care physicians only (OECD 2019).
Defined daily dose (DDD) is the assumed average dose per day for a drug when used for its main indication in adults (OECD 2021:156). DDDs do not necessarily reflect the true average daily dose used in a given country.
People with diabetes
Diabetes is a chronic condition marked by high levels of glucose in the blood. It is caused either by the inability to produce insulin (a hormone made by the pancreas to control blood glucose levels) or by the body not being able to use insulin effectively, or both.
Diabetes may result in a range of health complications, including heart disease, kidney disease, blindness and lower limb amputation. It is frequently associated with other chronic health conditions, such as cardiovascular disease and chronic kidney disease.
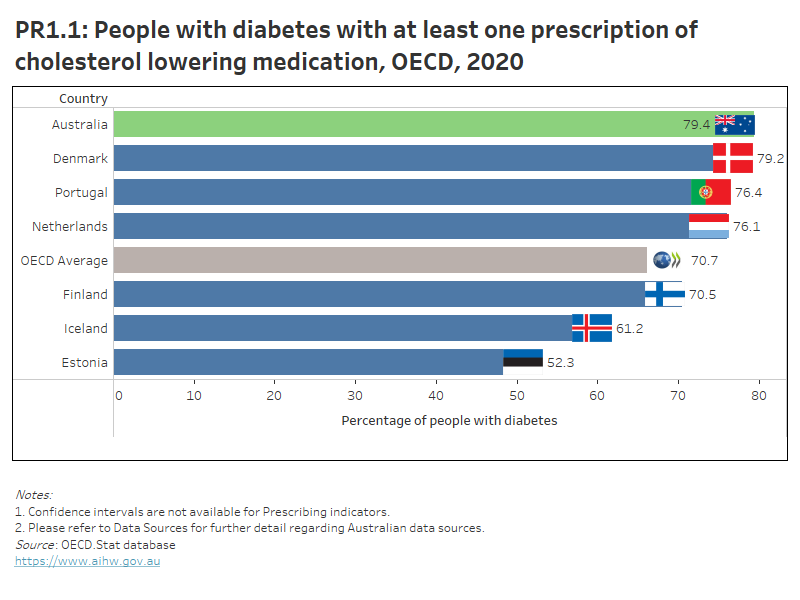
In Australia, 79% of people with diabetes were dispensed at least one prescription of cholesterol lowering medication in 2020 – the highest rate among OECD countries that submitted data. This percentage was higher for males (81%) than females (77%). The OECD average was 71%.
Interactive PR1.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR1.2 presents Australia’s 10-year trend for this indicator.
For people with diabetes and hypertension concurrently, angiotensin-converting enzyme inhibitors (ACE-Is) or angiotensin receptor blockers (ARBs) are recommended in most national guidelines as first-line medications for reducing blood pressure (OECD 2021).
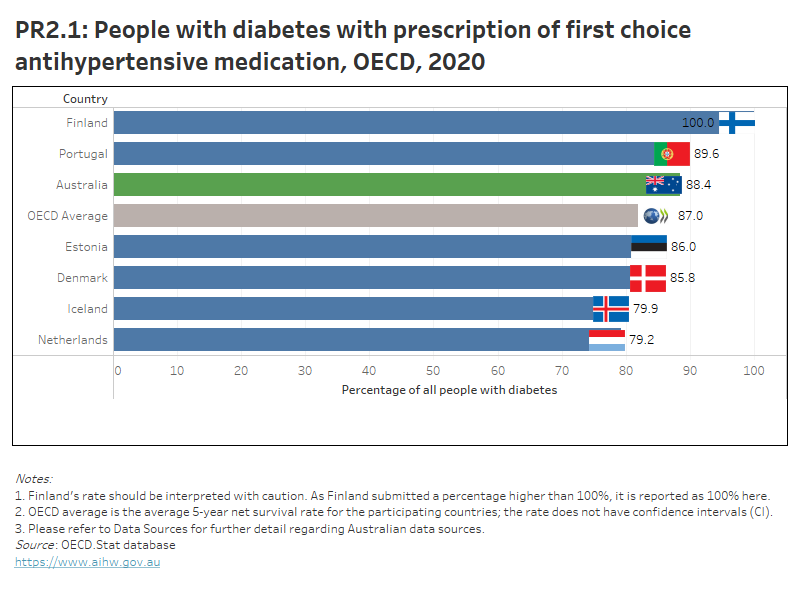
In Australia, 88% of people with diabetes were dispensed at least one prescription for a first-line antihypertensive medication in 2020. This percentage was higher for males (90%) than females (87%).
Australia had the third highest rate among OECD countries that submitted data, behind Finland (100%) and Portugal (90%). The OECD average was 87%.
Interactive PR2.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR2.2 presents Australia’s 10-year trend for this indicator.
PR1.1 presents OECD countries with data available for ‘people with diabetes with at least one prescription of cholesterol lowering medication’ indicator in 2020, which shows Australia had the highest rate. PR1.2 presents Australia’s 10-year trend for this indicator, which has remained between 78% and 82% since 2011.
PR2.1 presents OECD countries with data available for ‘people with diabetes with prescription of first choice antihypertensive medication’ indicator in 2020, which shows Australia had the 3rd highest rate. PR2.2 presents Australia’s 10-year trend for this indicator, which shows a gradual increase since 2013.
Refer to the data tables for more information.
Benzodiazepine use among older adults
Benzodiazepine is a type of sedative, a group of drugs that cause calming and sedative effects due to their depressive activity on the central nervous system. It is commonly prescribed for older adults with anxiety and sleep problems. However, long-term use of benzodiazepines can lead to adverse events such as falls, road accidents and overdose, tolerance, dependence and dose escalation (OECD 2017). However, long-acting benzodiazepines are not recommended for older adults as they take longer for the body to eliminate (OECD 2017). Older adults are defined as people aged 65 years and over.
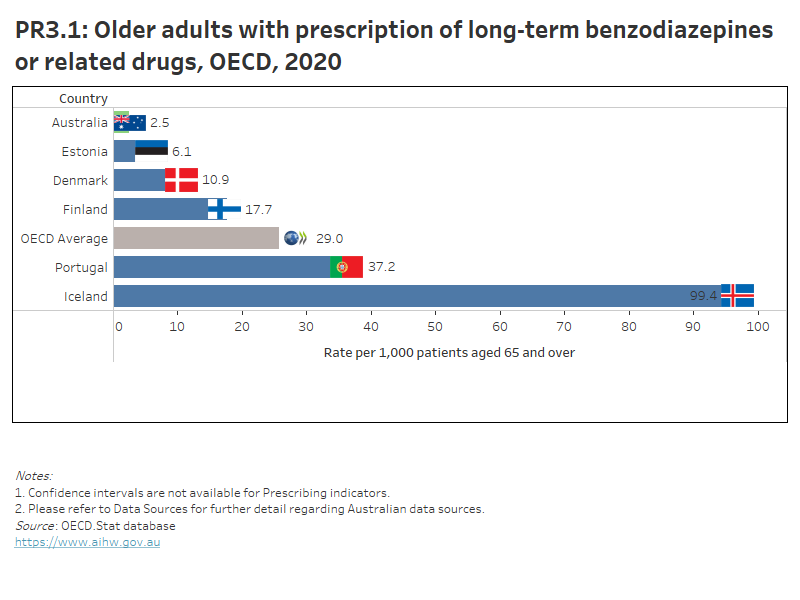
In Australia, 2.5 per 1,000 older adults were chronic benzodiazepine users (≥365 DDDs in one year) in 2020, a decrease from 7.0 per 1,000 older adults in 2011. The rate was higher for females than males (2.8 and 2.1 per 1,000 older adults, respectively), although the gap between males and females has narrowed over the past decade.
Australia had the lowest rate among OECD countries that submitted data. The OECD average was 29 per 1,000 older adults.
Interactive PR3.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR3.2 presents Australia’s 10-year trend for this indicator.
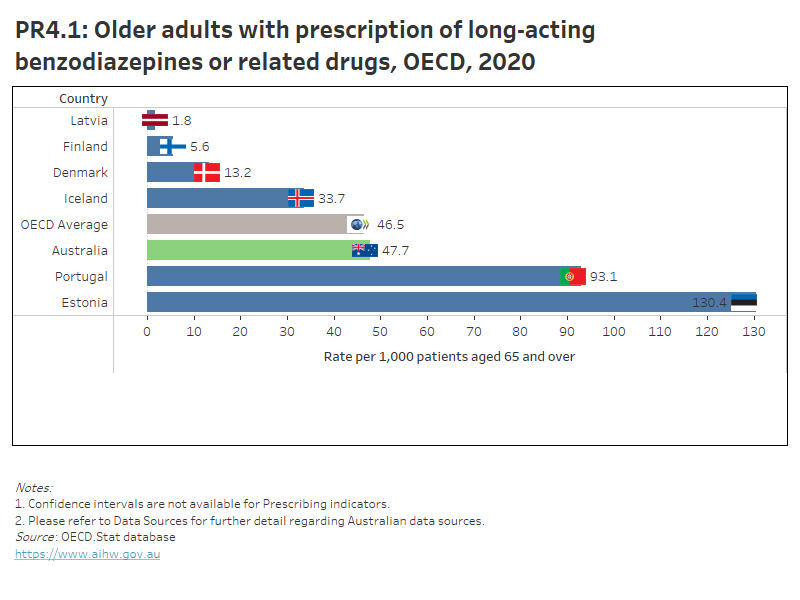
In 2020, 48 per 1,000 older adults in Australia were dispensed at least one prescription of long-acting benzodiazepines or related drugs, showing a decrease from 63 per 1,000 older adults in 2011. The rate was higher for females than males (57 and 37.5 per 1,000 older adults, respectively).
The OECD average was 47 per 1,000 older adults, and Latvia had the lowest rate (1.8 per 1,000 older adults).
Interactive PR4.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR4.2 presents Australia’s 10-year trend for this indicator.
PR3.1 presents OECD countries with data available for ‘Older adults with prescription of long-term benzodiazepines or related drugs’ indicator in 2020, which shows Australia had the lowest rate. PR3.2 presents Australia’s 10-year trend for this indicator, which shows an overall decrease since 2011.
PR4.1 presents OECD countries with data available for ‘Older adults with prescription of long-acting benzodiazepines or related drugs’ indicator in 2020, which shows Australia had a similar rate to the OECD average. PR4.2 presents Australia’s 10-year trend for this indicator, which shows an overall decrease since 2011.
Refer to the data tables for more information.
Antipsychotic use among older adults
People with dementia may experience changed behaviours, such as aggression, agitation and delusions, commonly known as behavioural and psychological symptoms of dementia. To manage these symptoms, non-pharmacological interventions are recommended, but medical professionals may prescribe antipsychotics to people with behavioural and psychological symptoms of dementia as a last resort. However, inappropriate prescribing of antipsychotic medicines may be a problem among older people living in residential aged care and was a key issue raised in the Royal Commission into Aged Care Quality and Safety (Royal Commission 2021). Older people are defined as people aged 65 years and over.
In Australia, 33 per 1,000 older adults were prescribed antipsychotics in 2020 – a decrease from 40 per 1,000 older adults in 2011. Females were more likely to be prescribed antipsychotics than males (35 and 31 per 1,000 population, respectively).
The OECD average was 42 per 1,000 older adults, and Latvia had the lowest rate (4.8 per 1,000 older adults).
Interactive PR5.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR5.2 presents Australia’s 10-year trend for this indicator.
PR5.1 presents OECD countries with data available for ‘Proportion of older adults prescribed antipsychotics’ indicator in 2020, which shows Australia had a lower rate than the OECD average. PR5.2 presents Australia’s 10-year trend for this indicator, which shows a gradual decrease from 2011.
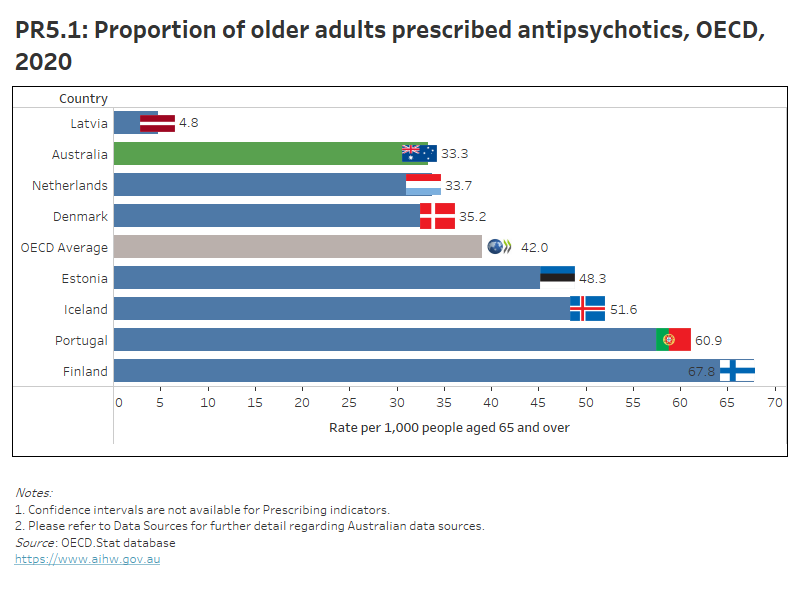
Refer to the data tables for more information.
Polypharmacy among people aged 75 years and over
Polypharmacy is the use of multiple medications concurrently. The OECD indicator measures the proportion of people aged 75 years and over who are taking more than five medications concurrently. Although polypharmacy is often necessary for people with many chronic health conditions, it increases the risk of medicines-related harm because of the greater chance of drug interaction and making mistakes with medicines (ACSQHC 2021).
In Australia, 40% of people aged 75 and over took more than five medications concurrently in 2020. The trend has remained relatively stable since 2016. The gap between males and females has narrowed over the past decade, with the two groups having similar rates (41% and 40%, respectively) in 2020.
Australia’s rate was lower than the OECD average of 42%, and Denmark had the lowest rate (22%).
Interactive PR6.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR6.2 presents Australia’s 10-year trend for this indicator.
PR6.1 presents OECD countries with data available for ‘Polypharmacy among people aged 75 and over’ indicator in 2020, which shows Australia had a lower rate than the OECD average. PR6.2 presents Australia’s 10-year trend for this indicator, which has remained between 40% and 41% since 2016.
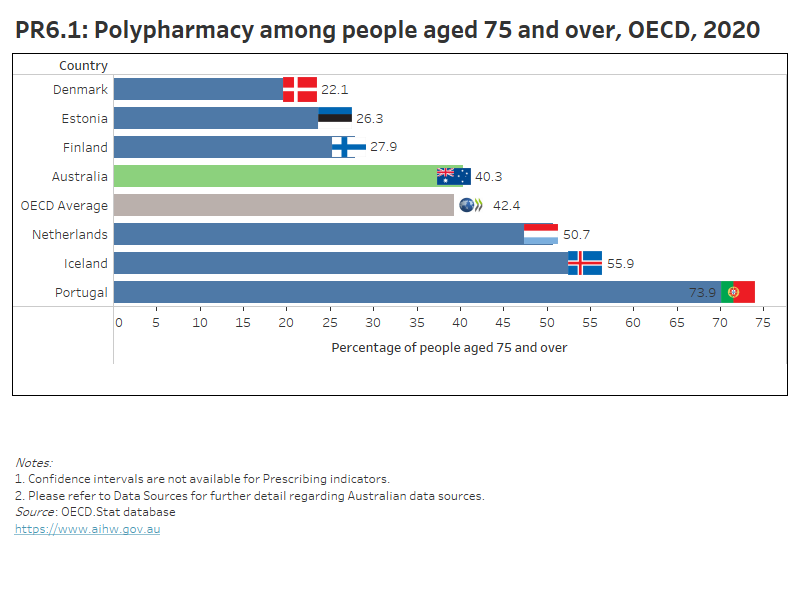
Refer to the data tables for more information.
Long-term prescription of anticoagulants in combination with an oral non-steroidal anti-inflammatory drug
Anticoagulants are medicines that prevent or reduce the risk of blood clotting, such as warfarin. NSAIDs are widely used medications for treating pain, inflammation and fever, such as aspirin and ibuprofen. The concurrent use of anticoagulants and NSAIDs can increase the risk of major bleeding and stroke (Kent et al. 2018).
In Australia, 11 per 100 long-term users of anticoagulants had at least one prescription of NSAID dispensed in 2020. The rate has decreased from 14 per 100 long-term users of anticoagulants in 2013, but is similar to the rate seen in 2011. The rate in 2020 was similar for males and females (11 per 100 long-term users of anticoagulants).
Among OECD countries that submitted data, the OECD average was 12 per 100 long-term users of anticoagulants, and Finland had the lowest rate (5.4 per 100 long-term users of anticoagulants).
Interactive PR7.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR7.2 presents Australia’s 10-year trend for this indicator.
PR7.1 presents OECD countries with data available for ‘Long-term prescription of anticoagulants in combination with an oral non-steroidal anti-inflammatory drug’ indicator in 2020, which shows Australia had a similar rate to the OECD average. PR7.2 presents Australia’s 10-year trend for this indicator, which shows a decrease since 2014.
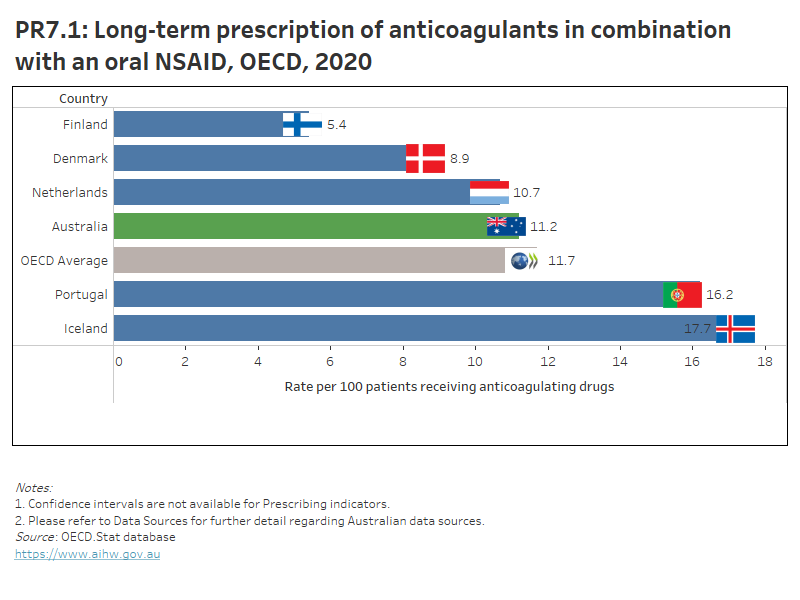
Refer to the data tables for more information.
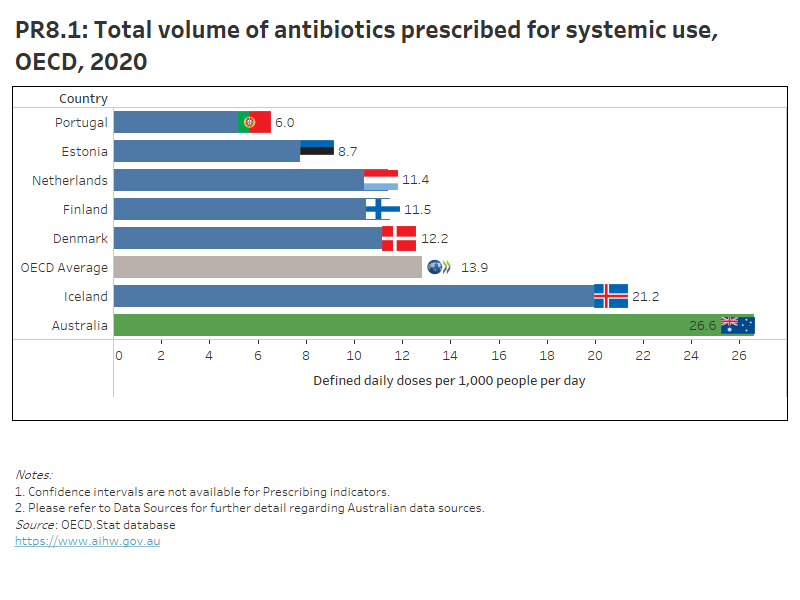
Antibiotic use
Antibiotics are medicines that destroy or slow the growth of bacteria. They are often prescribed to treat infection sites and infected wounds. However, unnecessary prescribing of antibiotics can increase anti-microbial resistance within the population (AIHW 2018a).
Australia’s total volume of antibiotics prescribed in primary care in 2020 was 27 DDD/1,000 people/day, the highest rate among OECD countries that submitted data. The OECD average was 14 DDD/1,000 people/day, and Portugal had the lowest rate of 6 DDD/1,000 people/day.
Australia’s rate has fluctuated over time in the past decade, ranging between 34 DDD/1,000 people/day in 2014 and 2015 to 27 in 2020. Females were more likely to be prescribed antibiotics than males (29 and 23 DDD/1,000 people/day, respectively).
Interactive PR8.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR8.2 presents Australia’s 10-year trend for this indicator.
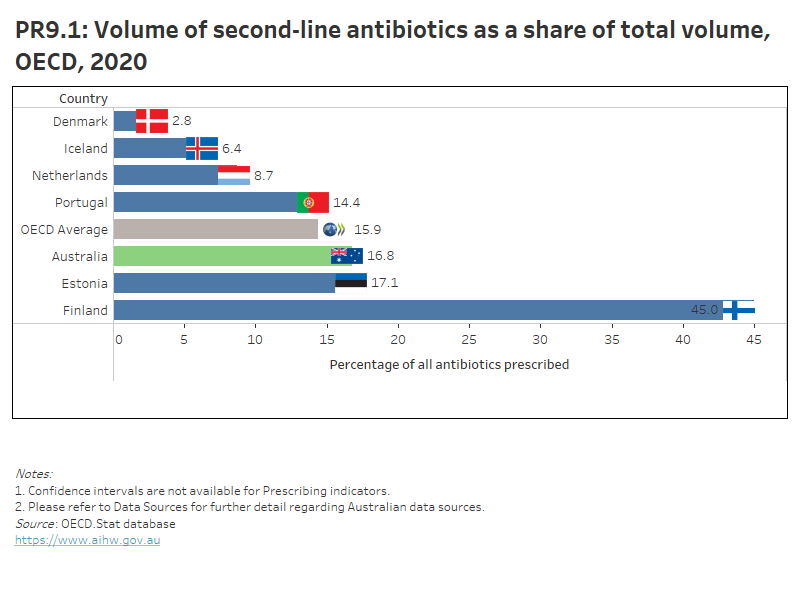
Meanwhile, the volume of second-line antibiotics comprised 17% of the total volume of antibiotics prescribed in Australia in 2020. Second-line antibiotics are antibiotics that are given when the initial prescription of antibiotics was not effective. The trend has remained relatively stable, ranging between 15% to 17% since 2012. The rate was similar for males and females (around 17%).
Australia’s rate was close to the OECD average of 16% and Denmark had the lowest rate (3%).
Interactive PR9.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR9.2 presents Australia’s 10-year trend for this indicator.
PR8.1 presents OECD countries with data available for ‘Total volume of antibiotics for systemic use’ indicator in 2020, which shows Australia had the highest rate. PR8.2 presents Australia’s 10-year trend for this indicator, which shows a fluctuating trend over time.
PR9.1 presents OECD countries with data available for ‘Volume of second line antibiotics as a share of total volume’ indicator in 2020, which shows Australia had a similar rate to the OECD average. PR9.2 presents Australia’s 10-year trend for this indicator, which has remained between 15% and 17% since 2012.
Refer to the data tables for more information.
Opioid use
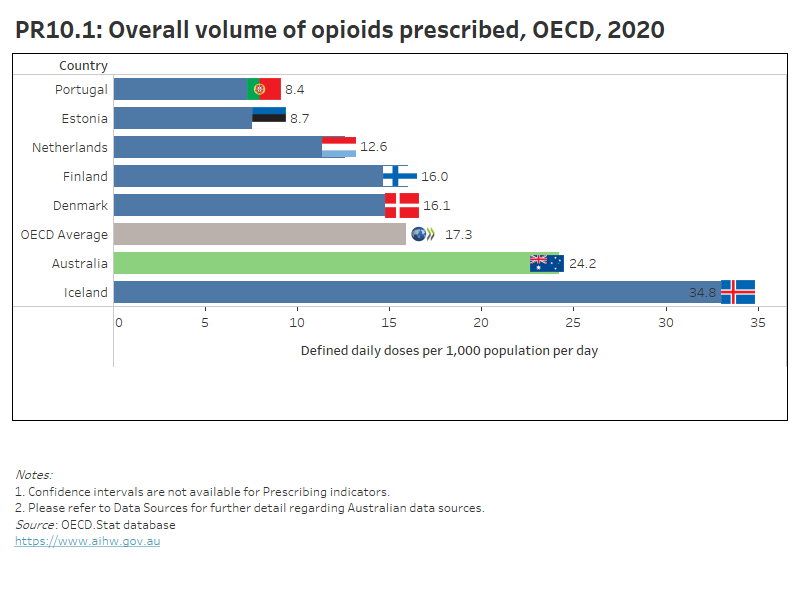
Opioids are chemical substances that have a morphine-type action in the body. They are commonly prescribed for pain relief, but can lead to dependence, breathing difficulties, and death (OECD 2019). Opioid drugs can be obtained either illicitly or via prescription. Legal or pharmaceutical opioids (including codeine and oxycodone) are responsible for significantly more deaths and poisoning hospitalisations than illicit opioids (such as heroin) (AIHW 2018b).
In Australia, the overall volume of opioids prescribed in primary care for people aged 18 and over in 2020 was 24 DDD/1,000 people/day – a decrease from 31 DDD/1,000 people/day in 2012. The rate was similar for males and females (around 24%).
The OECD average was 17 DDD/1,000 people/day. Portugal had the lowest rate (8 DDD/1,000 people/day).
Interactive PR10.1 below compares OECD countries that submitted data for 2020 for this indicator, while PR10.2 presents Australia’s 10-year trend for this indicator.
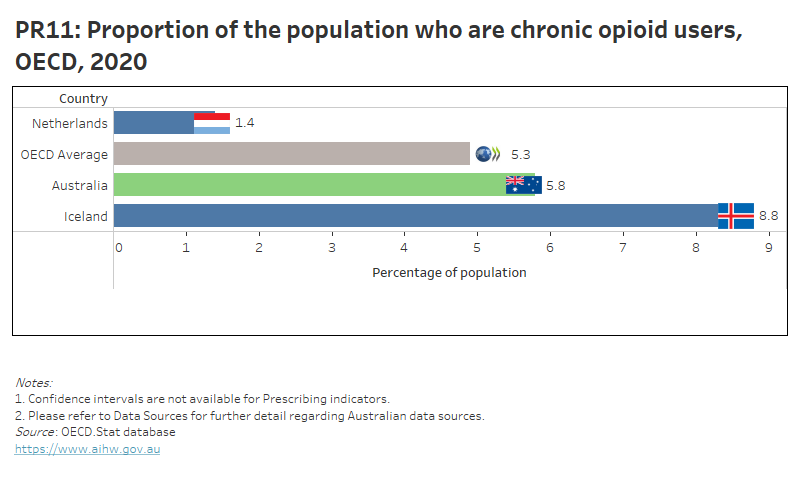
In the same period, 5.8% of Australia’s adult population were chronic users of opioids. The proportion was similar for males and females (5.4% and 6.0%, respectively). This was the first year Australia submitted data for this indicator, and only three OECD countries submitted data for this indicator for 2020 (PR11).
PR10.1 presents OECD countries with data available for ‘Overall volume of opioids prescribed’ indicator in 2020, which shows Australia had a higher rate than the OECD average. PR10.2 presents Australia’s 10-year trend for this indicator, which shows a gradual decrease since 2012.
PR11 presents the three OECD countries with data available for ‘Proportion of the population who are chronic opioid users’ indicator in 2020.
Refer to the data tables for more information.
ACSQHC 2021. 6.1 Polypharmacy, 75 years and over. Sydney: ACSQHC. Viewed 28 September 2021.
AIHW 2018a. Australia’s health 2018. Australia’s health series no. 15. Cat. no. AUS 221. Canberra: AIHW.
AIHW 2018b. Opioid harm in Australia: and comparisons between Australia and Canada. Cat . no. HSE 210. Canberra: AIHW.
Kent AP, Brueckmann M, Fraessdorf M et al. 2018. Concomitant oral anticoagulant and nonsteroidal anti-inflammatory drug therapy in patients with atrial fibrillation. Journal of the American College of Cardiology 72(3):255–267.
OECD 2017. Health at a glance 2017: OECD indicators. Paris: OECD.
OECD 2019. Health at a glance 2019: OECD indicators. Paris: OECD.
OECD 2021. Health at a glance 2021: OECD indicators. Paris: OECD.
Royal Commission (Royal Commission into Aged Care Quality and Safety) 2021. Final report: Care, Dignity and Respect. Volume 1 Summary and recommendations.


