Technical notes
Data on health service use from datasets in the National Integrated Health Services Information Analysis Asset (NIHSI AA) were used to estimate health service use and costs for Australians in their last year of life. This section presents the methods for estimating the number of health services used, and corresponding costs.
About the National Integrated Health Services Information Analysis Asset
The NIHSI AA is an enduring linked data asset managed under the custodianship of the AIHW. It is available for analysis by the AIHW and participating jurisdictions for approved projects.
Data on service use, costs and deaths from the first iteration of NIHSI AA (version 0.5) were used to estimate health service use and calculate associated costs. Key datasets in the NIHSI AA version 0.5 used in this analysis were:
- National Death Index (NDI), which contains person-level cause of death information previously linked from the National Mortality Database (AIHW 2021a)
- National Medicare Benefits Schedule (MBS)
- National Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Benefits Scheme (RPBS)
- Residential aged care data from the National Aged Care Data Clearinghouse
- Admitted patient care from the National Hospital Morbidity Database for public hospitals in New South Wales, Victoria, South Australia and Tasmania and some private hospitals in Victoria
- Non-Admitted Patient Emergency Department Care National Minimum Data Set for public hospitals in New South Wales, Victoria, South Australia, Tasmania.
Data was available between 1 July 2010 and 30 June 2017 for most datasets, except for deaths data which was available up to 31 December 2017.
NIHSI AA population and study groups
Overall, just under 26 million people were identified in the NIHSI AA version 0.5 (hereafter referred to as NIHSI AA) from records between 1 July 2010 and 31 December 2017. This is based on the Medicare Consumer Directory, a database of people enrolled in Medicare used in the creation of NIHSI AA, combined with 3 other main datasets – NDI, residential aged care data and hospitals data (admitted patient and emergency department care). All people in the Medicare Consumer Directory were first identified, which accounted for 97.8% of the NIHSI AA population. People not in the Medicare Consumer Directory but who appeared in hospital datasets accounted for an additional 2%. Those in the NDI and residential aged care data accounted for the remainder.
Study groups
In this study, the NIHSI AA population was divided into 2 study groups:
- People in the last year of life – includes people who had a death record in the NDI data between 1 July 2010 and 31 December 2017. Health service use in the 12 months before death was examined for each person and associated costs calculated.
- People not in the last year of life – includes people who did not have a death record in the NDI data between 1 July 2010 and 31 December 2017. Health service use between 1 July 2010 and 31 December 2016 was examined for each person and associated costs calculated.
The NIHSI AA comprises 4 core health and aged care service data (MBS, PBS/RPBS, residential aged care and hospital care) and deaths data (from the NDI). It therefore excludes people who did not use any of these services and/or did not have a death record in the NDI data at any point during the study period. Table A1 shows the numbers and proportions of the NIHSI AA population within each study group. Approximately 4% of people identified in the data were in their last year of life and 96% not in their last year.
Table A1: Cumulative population and percentage in each study group from records in NIHSI AA version 0.5
| Study group(a) | Total | Per cent (%) |
| People in the last year of life | 1,137,043 | 4.4 |
| People not in the last year of life | 24,736,845 | 95.6 |
| Total population in NIHSI AA | 25,873,888 | 100.0 |
(a) Population in scope are people identified in the National Integrated Health Services Information Analysis Asset version 0.5. The ‘last year of life’ group includes people who died between 1 July 2010 and 31 December June 2017. People not in the last year of life includes people without a death record between 1 July 2010 and 31 December 2017.
People in the last year of life
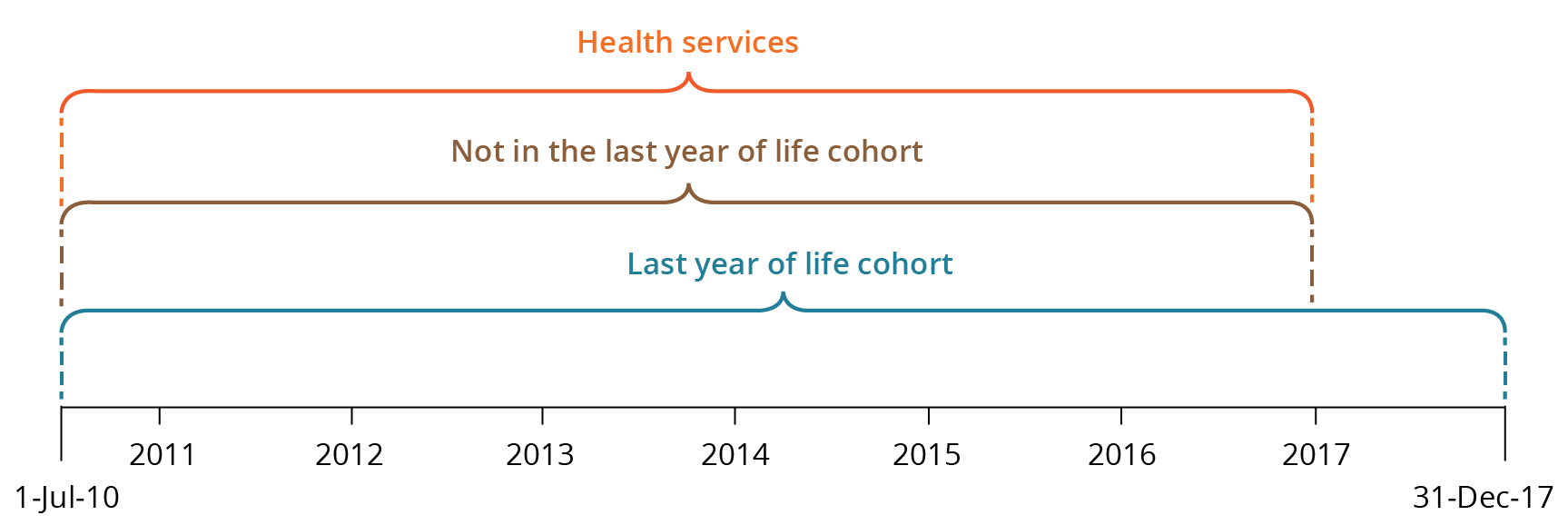
Health service use in the 12 months before death was retrospectively examined for people in their last year of life. Note that for health service use and costs for people who died in the first year of data, the study period will not cover a full 12 months before death. As a result, health service use and costs for people in their last year of life may be slightly underestimated. Figure A1 shows the time periods for the study cohorts and service use in scope.
People not in the last year of life
The number of health services used over the study period was examined for people not in their last year of life. Unlike the last-year-of-life group, which covers 7.5 years of NIHSI AA data, the study period for people not in the last year of life covers 6.5 years of data (between 1 July 2010 and 31 December 2016). For people not in the last year, service use between 1 January 2017 and 31 December 2017 was excluded because those who died in the following 12 months could not be identified.
Although the study periods for these 2 population groups are slightly different, they are mutually exclusive and useful comparisons can be made between the average number of health services used and associated costs for each group over 12 months.
Figure A1: Time period for study groups (whether in last year of life or not) and health service use
Identifying people who used residential aged care services
Health service use and costs over the study period (between 1 July 2010 and 31 December 2016) were disaggregated by whether a person used residential aged care services or not. This includes people living in permanent residential care and/or those who stayed one or more days in respite care over the study period.
Four comparison populations were derived:
1. People in the last year of life
- people who used residential aged care at any point during their last year of life
- people who did not use residential aged care in their last year of life
2. People not in the last year of life
- people who used residential aged care at any point during the study period
- people who did not use residential aged care during the study period.
Residential aged care data were only used to indicate whether people had used residential aged care or not. The care and support provided by residential aged care services directly are not captured in the 4 health service types examined.
Estimating age
The age of people in the study groups was based on when the person died and when they used a health or aged care service. These dates were used to first estimate single year ages of each person in the study groups.
For people in the last year of life, age at death was calculated by adjusting each person’s age at their first service in the linked data, by half a year. For example, if a person was recorded as being aged 84 at their first service, it was estimated that they were 84.5 years old, because there was no information on the number of days since their 84th birthday. Then the difference in years between the first service and when the person died was added to the adjusted age to derive single year of age for each person in their last year of life. For example, if the difference in years was
6.5 years, then the person was aged 91 when they died (84.5 years plus 6.5 years).
For people not in the last year of life, adjusted age at first linked service was added to the difference in years between the first and the last service used.
For people in the last year of life, information on the person’s sex and age at death was obtained from the NDI data because this was considered the most accurate source. For people not in their last year of life, information on the person’s sex and age at first service was obtained from other data sources.
For reporting purposes, health service use and cost estimates are reported in 10-year or broader age groups.
Estimating health service use and costs
The study examined 4 health service types: emergency department (ED) presentations; hospital admissions; MBS services; and prescriptions supplied under the PBS/RPBS. Different approaches were used to estimate costs and number of health services used by people in their last year of life and those not in their last year between July 2010 and December 2016.
Calculating National Weighted Activity Units for acute admitted hospital and ED services
The first approach involved calculating the National Weighted Activity Units (NWAUs) to derive a common unit against which costs can be applied for hospital use. NWAU is a measure of health service activity expressed as a common unit, against which the National Efficient Price (NEP) is paid. NWAU is a way of comparing and valuing each public hospital service (whether ED presentations, admissions or outpatient episodes), weighted for clinical complexity. NWAUs were calculated for acute admitted services and ED presentations. In this report, acute admitted services include mental health admissions. For more information on NWAUs see: https://www.publichospitalfunding.gov.au/calculation-national-weighted-activity-unit
Historical hospital utilisations of service categories (acute admitted and ED presentations), except for subacute, considered to have been funded under activity-based funding between 1 July 2010 and 31 December 2016 were converted into NWAUs. This was done using the Independent Hospital Pricing Authority (IHPA) NWAU16 calculators for acute admitted services and ED presentations.
NWAU16 calculators were selected as the most appropriate bases for standardising hospital uses because at the time of this analysis, the latest data available in NIHSI AA were for 2016–17 and for only 4 jurisdictions (New South Wales, Victoria, South Australia, and Tasmania). In addition, the IHPA 2016–17 NEP was selected and applied to estimate the cost of hospital utilisations. However, the AIHW has since updated the NIHSI AA (to version 1.0) to include 2018–19 data and for 6 jurisdictions (New South Wales, Victoria, South Australia, Tasmania, Queensland and the Australian Capital Territory).
To account for clinical complexity, NWAUs were derived at episode level by applying price weights and adjustments developed by the IHPA. Price weights for NWAU16 used include:
- Diagnostic Related Groups for acute admitted services
- Urgency Related Groups or Urgency Disposition Groups for ED presentations.
Adjustments for Indigenous status, radiotherapy, dialysis, and paediatric services were applied to acute admitted services and ED presentations to create a consistent, uniform set of service utilisations and costs, comparable across care types. For more information on IHPA’s NWAU16 calculators see: National Efficient Price Determination 2016-17 and Technical Specifications.
NWAUs derived in this study were compared with those published by the Administrator for 2015–16 and 2016–17. They were found to be slightly higher than those supplied by jurisdictions to the Administrator for payment purposes. This is because costs calculated for this study include the most recent data available.
After calculating NWAUs, the cost of hospital services (for acute admitted services and ED presentations) were calculated by multiplying the volume of weighted services by the 2016–17 NEP ($4,883 per NWAU). For more information see: IHPA’s determinations of the National Efficient Price is available in the National Efficient Price Determination 2016–17.
The costs estimated using this approach did not consider proportions of Australian Government and state and territory government contributions. Since the costs estimated are at national level, cross-border adjustments were not considered.
Estimating MBS services and prescriptions supplied under the PBS/RPBS
The second approach involved estimating the number of MBS services and number of prescriptions supplied under the PBS and RPBS, and their associated costs.
MBS items were mapped to broad type of service categories to obtain the total MBS services and total costs by broad type of service, such as un-referred (GP) attendances, specialist attendances and operations (Table A2). Fee charged, including patient co-payment, were used as the total cost of an MBS service. These estimates should be interpreted with caution due to data limitations that may have underestimated or overestimated the total cost of MBS services.
| Broad Type of Service items | MBS item |
| Unreferred attendances: VR GP | 1:4, 13:14, 19:20, 23:26, 33, 35:40, 43:44, 47:51, 193, 195, 197, 199, 597, 599, 601:603, 2497:2501, 2503:2504, 2506:2507, 2509, 2517:2518, 2521:2522, 2525:2526, 2546:2547, 2552:2553, 2558:2559, 2574:2575, 2577:2578, 5000, 5003, 5007, 5010, 5020:5023, 5026:5028, 5040:5043, 5046, 5049, 5060, 5063:5064, 5067 |
| Unreferred attendances: enhanced primary care | 700:710, 712:747, 749:750, 757:759, 762, 765, 768, 771:773, 775, 778:779, 900, 903, 2700:2702, 2710, 2712:2713, 2715, 2717, 2719, 6087 |
| Unreferred attendances: other | 5:12, 15:18, 21:22, 27:32, 34, 41:42, 45:46, 52:84, 86:87, 89:93, 95:98, 101, 160:173, 444:449, 598, 600, 696:698, 980, 996:998, 2100, 2122, 2125:2126, 2137:2138, 2143, 2147, 2179, 2195:2199, 2220, 2598, 2600, 2603, 2606, 2610, 2613, 2616, 2620, 2622:2624, 2631:2633, 2635, 2664, 2666:2668, 2673:2675, 2677, 2704:2705, 2707:2708, 2721, 2723, 2725, 2727, 4001, 5200, 5203, 5207:5208, 5220:5228, 5240, 5243, 5247:5248, 5260:5263, 5265:5267, 17600 |
| Practice nurse | 711, 10983:10984, 10986:10989, 10993:10999 |
| Specialist | 85, 88, 94, 99:100, 102:152, 154:159, 288:289, 291:293, 296:297, 299:338, 342:353, 355:359, 361, 364, 366:367, 369:370, 384:389, 410:417, 501:503, 507, 511, 515, 519:520, 530, 532, 534, 536, 801, 803, 805, 807:809, 811:813, 815, 820, 822:823, 825:830, 832, 834:835, 837:838, 851:852, 855, 857:858, 861, 864, 866, 871:872, 880, 887:893, 2799, 2801, 2806, 2814, 2820, 2824, 2832, 2840, 2946:2949, 2954, 2958, 2972:2978, 2984:3003, 3005, 3010, 3014:3015, 3018, 3023, 3028:3032, 3040, 3044, 3051:3055, 3062, 3069, 3074:3078, 3083, 3088, 3093, 5906:5912, 6004, 6007:6009, 6011:6016, 6018:6019, 6023:6026, 6028:6029, 6031:6032, 6034:6035, 6037:6038, 6042, 6051:6052, 6057:6060, 6062:6065, 6067:6068, 6071:6075, 6080:6081, 10801:10816, 17603:17690 |
| Diagnostic imaging | 791:794, 910:911, 913, 990:993, 995, 999, 2400:2460, 2502, 2505, 2508, 2512:2516, 2520, 2524, 2528:2545, 2548:2551, 2554:2557, 2560:2573, 2576, 2579:2597, 2599, 2601, 2604, 2607:2609, 2611, 2614, 2617, 2621, 2625:2630, 2634, 2638:2657, 2665, 2672, 2676, 2678:2699, 2703, 2706, 2709, 2711, 2714, 2716, 2718, 2720, 2722, 2724, 2726, 2728:2798, 2800, 2802:2805, 2807:2813, 2815:2819, 2823, 2825:2831, 2833:2839, 2841:2859, 2960:2971, 2980:2981, 5861, 8712:8713, 8716:8717, 8720:8721, 8723:8724, 8727:8849, 8851:8874, 9066, 9341:9344, 55000:55054, 55056:64991 |
| Pathology collection | 73899:73940, 74992:74999 |
| Pathology tests | 1001:2099, 2101:2120, 2123:2124, 2127:2136, 2139:2142, 2145:2146, 2148:2178, 2181:2192, 2201:2219, 2221:2399, 65001:73844, 74990:74991 |
| Other allied health services | 10950:10977, 80000:82035, 82300:87777 |
| Obstetrics | 190:192, 194, 196, 198, 200:284, 290, 295, 298, 354, 360, 362:363, 365, 368, 383, 9011, 15999, 16399:16636 |
| Anaesthetics | 401:409, 443, 450:500, 505:506, 509:510, 513:514, 517:518, 521:529, 531, 533, 535, 537:577, 748, 751:756, 760, 764, 767, 787:790, 9021:9042, 13006:13009, 17500:17506, 17701:18298, 20100:25205 |
| Operations | 924, 3004, 3006, 3012, 3016, 3022, 3027, 3033:3039, 3041, 3046:3050, 3058, 3063, 3073, 3082, 3087, 3092, 3098:3101, 3104:3113, 3116, 3120:3124, 3130, 3135:3142, 3148:3173, 3178:3183, 3194:3226, 3233:3237, 3247:3253, 3261:3265, 3271:3281, 3289, 3295:3330, 3332:3384, 3391, 3399, 3404:3425, 3431:3455, 3459, 3465, 3468:3472, 3477:3480, 3495:3496, 3505, 3509:3516, 3526:3988, 4012:4838, 4844:4860, 4864:4999, 5002, 5006, 5009, 5015:5018, 5024, 5029:5038, 5045, 5048, 5050:5059, 5062, 5066, 5068:5196, 5201, 5205, 5210:5217, 5229:5237, 5241:5242, 5245, 5254, 5264, 5268:5270, 5277:5280, 5284, 5288, 5292:5855, 5864:5905, 5916:6001, 6005:6006, 6010, 6017, 6022, 6027, 6030, 6033, 6036, 6039:6041, 6044:6050, 6053:6056, 6061, 6066, 6069:6070, 6077:6079, 6083:6086, 6089:6918, 6922:7126, 7129:7133, 7135:7143, 7147,7397, 7410:7483, 7505:7719, 7721:7722, 7725, 7727:7728, 7739:7743, 7749, 7764:7766, 7774:7803, 7808:7809, 7815:7817, 7821:7823, 7828, 7834, 7839, 7844:7847, 7853:7886, 7898:7902, 7911:8003, 8009:8173, 8179:8458, 8462, 8466:8467, 8470:8478, 8480:8481, 8483:8504, 8508:8512, 8515:8519, 8521:8557, 8560, 8564, 8568:8570, 8574, 8578, 8582:8636, 8640, 8644, 8648, 8652, 8655:8658, 8660, 8662, 8664, 8666, 8668, 8670, 8672, 8674:8699, 9401:9409, 9415:9435, 9438, 9441:9449, 9458, 9476:9478, 30000:30524, 30526:30632, 30634:41868, 41870:42824, 42833:50952 |
| Assistance at operations | 2951:2953, 2955:2957, 51300:51318 |
| Optometry | 180:186, 10900:10948 |
| Radiotherapy and Therapeutic Nuclear Medicine | 2861:2945, 8850, 8875:8886, 9381:9392, 15000:15900, 16000:16018 |
| Miscellaneous | 153, 340, 770, 774, 777, 780:786, 795:800, 802, 804, 806, 810, 814, 816:819, 821, 824, 831, 833, 836, 839:850, 853:854, 856, 859:860, 862:863, 865, 870, 874:879, 882:886, 895:897, 902, 904:909, 912, 915:923, 925:979, 981:989, 994, 3059, 3068, 3095, 3103, 3114, 3117, 3128, 3134, 3147, 3175, 3187, 3229:3230, 3245, 3258, 3268, 3284, 3290, 3331, 3386, 3393, 3400, 3427, 3456, 3462, 3466, 3475, 3483, 3500, 3507, 3521, 4003, 4841, 4862, 5249, 5259, 5274, 5282, 5286, 5291, 6920, 7128, 7134, 7146, 7402, 7485, 7720, 7723:7724, 7726, 7729:7731, 7745, 7753, 7770, 7804, 7812, 7818, 7824, 7831, 7836, 7841, 7849, 7888, 7907, 8006, 8175, 8460, 8464, 8468, 8479, 8482, 8506, 8514, 8520, 8558, 8562, 8566, 8572, 8576, 8580, 8638, 8642, 8646, 8650, 8654, 8659, 8661, 8663, 8665, 8667, 8669, 8671, 8673, 8700:8711, 8714:8715, 8718:8719, 8722, 8725:8726, 8901:8990, 9061:9065, 9067, 9410:9414, 9436:9437, 9439, 9450:9457, 9459:9475, 10985, 10990:10992, 11000:13003, 13012:14245, 18350:18379, 30525, 30633, 41869, 42827:42830, 51700:53706, 55055, 75000:75854, 82100:82225 |
Source: Department of Health 2022.
Similarly, listed items on the PBS/RPBS were mapped to Anatomical Therapeutic Chemical (ATC) groups to obtain the total number of prescriptions and associated costs by selected ATC groups. In this analysis, ATC3 groups, such as anti-dementia drugs, opioids and immuno-suppressants, were used. The total cost of prescriptions were calculated by adding benefits paid to patients’ contributions. However, this estimate is affected by data quality issues, including discounting of patient co-payment.
The 'Notes and caveats' section details data limitations and gaps for estimating the costs of MBS services and pharmaceuticals supplied under the PBS/RPBS.
Identifying cause of death
To estimate health service use and costs in the last year of life by cause of death, information on the underlying cause of death information in the NDI data was used. Two levels of groupings were included:
- cause of death disease group, based on the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) chapter level groupings (Table A3)
- ICD-10 codes for the 20 leading causes of death in Australia, based on the leading causes of death in Australia in 2019, and classified using an AIHW-modified version of Becker et al. 2006 (Table A4).
Disease groups with less than 15,000 deaths over the study period are not presented in the report’s data visualisations.
| Cause of death disease group in web report | ICD-10-Chapter disease group name | ICD-10 codes | Definition and examples of causes | Number of deaths |
| Infectious diseases | Certain infectious and parasitic diseases | A00–B99 | Includes diseases generally recognised as communicable or transmissible, such as intestinal infectious diseases, other bacterial diseases viral hepatitis and tuberculosis. | 19,707 |
| Cancer | Neoplasms | C00–D48 | Includes malignant neoplasms such as colorectal, pancreatic, lung, breast and prostate cancers. Also includes in situ and benign neoplasms, as well as neoplasms of uncertain or unknown behaviour. | 334,675 |
| Endocrine diseases (including diabetes) | Endocrine, nutritional and metabolic diseases | E00–E90 | Includes diabetes mellitus, disorders of the thyroid gland, malnutrition, obesity, and metabolic disorders. | 46,505 |
| Mental and behavioural disorders | Mental and behavioural disorders | F00–F99 | Includes disorders of psychological development such as schizophrenia, mental and behavioural disorders due to psychoactive substance use, mood disorders and some but not all types of dementia. Does not include suicide and self-harm, which is included under External causes. | 92,221 |
| Nervous system diseases | Diseases of the nervous system | G00–G99 | Includes diseases such as epilepsy, muscular dystrophy, spinal muscular atrophy, Alzheimer's disease, and inflammatory diseases of the central nervous system. | 32,059 |
| Cardiovascular diseases | Diseases of the circulatory system | I00–I99 | Includes diseases such as coronary heart disease, cerebrovascular disease, heart failure, hypertensive disease and cardiac arrhythmias. | 330,594 |
| Respiratory diseases | Diseases of the respiratory system | J00–J99 | Includes diseases such as chronic obstructive pulmonary disease (COPD), influenza and pneumonia. | 102,791 |
| Digestive diseases | Diseases of the digestive system | K00–K93 | Includes diseases such as diseases of the liver and intestines. | 40,967 |
| Genitourinary diseases | Diseases of the genitourinary system | N00–N99 | Includes diseases such as kidney failure and diseases of the urinary system. | 25,898 |
| External causes (Injury and poisoning) | External causes of morbidity and mortality | V01–Y98 | Includes external causes of injuries such as accidents, falls and assaults, as well as suicide and poisoning. | 73,204 |
| Other | Other ICD-10 chapters | Includes: D50–D89, H00–H59, H60–H95, L00–L99, M00–M99, O00–O99, P00–P96, Q00–Q99, R00–R99 |
Includes Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50–D89), Diseases of the eye and adnexa (H00–H59), Diseases of the ear and mastoid process (H60-H95), Diseases of the skin and subcutaneous tissue (L00–L99), Diseases of the musculoskeletal system and connective tissue (M00–M99), Pregnancy, childbirth and the puerperium (O00-O99), Certain conditions originating in the perinatal period (P00–P96), Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) and Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99). | 38,422 |
| Total | All Chapter level causes | 1,137,043 |
Source: AIHW National Integrated Health Services Information Analysis Asset version 0.5.
| Rank(a) | Cause of death | Number of deaths |
| 1 | Coronary heart disease (I20–I25) | 148,972 |
| 2 | Dementia (including Alzheimer’s disease) (F01, F03, G30) | 86,773 |
| 3 | Cerebrovascular disease (I60–I69) | 79,883 |
| 4 | Lung cancer (C33, C34) | 61,340 |
| 5 | Chronic obstructive pulmonary disease (COPD) (J40–J44) | 49,836 |
| 6 | Colorectal cancer (C18–C20, C26.0) | 38,969 |
| 7 | Diabetes (E10–E14) | 33,225 |
| 8 | Influenza and pneumonia (J09–J18) | 22,443 |
| 9 | Prostate cancer (C61) | 23,773 |
| 10 | Heart failure and complications and ill-defined heart disease (I50–I51) | 25,833 |
| 11 | Suicide (X60–X84) | 20,446 |
| 12 | Breast cancer (C50) | 21,614 |
| 13 | Pancreatic cancer (C25) | 19,732 |
| 14 | Cancer of unknown or ill-defined primary site (C26, C39, C76–C80 excl. C26.0) | 20,391 |
| 15 | Accidental falls (W00–W19) | 16,987 |
| 16 | Kidney failure (N17–N19) | 17,062 |
| 17 | Other ill-defined causes (R00–R94, R96–R99, I46.9, I95.9, I99, J96.0, J96.9, P28.5) | 12,066 |
| 18 | Cardiac arrhythmias (I47–I49) | 15,060 |
| 19 | Liver cancer (C22) | 12,406 |
| 20 | Hypertensive disease (I10–I15) | 15,683 |
| 21 | All other causes | 394,549 |
| All Causes | 1,137,043 |
(a) Ranking is based on 2019 deaths, classified using the AIHW-modified version of Becker et al. 2006 causes of death classification.
Source: AIHW National Integrated Health Services Information Analysis Asset version 0.5.
Estimating health service use and associated costs
For each study group, the number of health services used and associated costs were first calculated over the study period. For the last year of life group, the period refers to the number of services used in the last 12 months of life for each person who died between 1 July 2010 and 31 December 2017. For the not in the last year of life group, the period refers to the number of services used between 1 July 2010 and 31 December 2016.
This was then averaged by the number of years examined (7.5 years for people in the last year of life and 6.5 years for those not in the last year) and the number of people in each group to obtain average annual health service use and costs per person.
Reporting average annual estimates per person provided a fair comparison measure between the 2 groups. Where appropriate, these measures were adjusted to account for differences in age structure.
Estimating lifetime health system costs
Estimating lifetime health system costs of Australians using the NIHSI AA is challenging because it does not include the full use of health services over a person’s lifetime. Hence, it was assumed that the use of health services and associated costs for people not in the last year of life was equivalent to the period before the 12 months before deaths for those in the last year of life. This methodology is a work in progress as the AIHW continues to revise this method.
For people in the last year of life, health service costs were divided into 2 groups (one to 6 months before death and
7 to 12 months before death). Costs per person by age and sex for each group were calculated by dividing total costs for people in the last year of life by the population in the last year of life.
To estimate health system costs incurred before the last year of life, annual age-specific costs by sex for people not in the last year were used. Since health system costs before the last year of life differ by age, the cumulative costs for each age group were estimated by applying the age difference to costs per person. Total lifetime costs by age group and sex were then derived by adding estimated costs in the one to 6 months before death and costs in the 7 to 12 months before death to the estimated costs before the last year of life.
Notes and caveats
Health services used by people in the last year of life outside of the 12 months before death were excluded from the study. They were not included in with people not in the last year of life. This may result in a slight underestimate of the number of services and costs for people not in their last year of life, particularly those with chronic health conditions who use multiple services.
Cost estimates were not adjusted for inflation.
Costs for hospital admissions and ED presentations
Costs for hospital admitted patient and ED presentations include Australian Government and state and territory government costs only. Non-government costs, such as out-of-pocket and private health insurance – estimated to represent around 21% of total spending on hospitals (Table 29, AIHW 2021b) – are not captured. Other health system costs not captured in the NIHSI AA and/or not included in estimates presented in this analysis are outlined in ‘Health services and costs excluded from the analysis’ under Study background.
Hospital utilisations and estimates of adjusted costs between 1 July 2010 and 31 December 2016 are of public hospital data and, where available, private hospitals and ED presentations in public hospitals for New South Wales, Victoria, South Australia and Tasmania.
Acute care type of newborn with unqualified days only have been excluded from estimates for acute admitted hospitalisations. Except for acute admitted (using care types 7.1 and 7.2 qualified days), it was not possible – using the information available – to estimate with certainty, separate and reliable perinatal (including neonatal) utilisations and costs. As such, their utilisations and costs have been included in the 0–9 age group.
MBS services and prescriptions supplied under the PBS
Health service costs for MBS services and prescriptions supplied under the PBS/RPBS include Australian Government benefits paid and patient out-of-pocket costs.
Total MBS and total PBS/RPBS estimated costs need to be interpreted with care. For the MBS this is because:
- Where a patient claims on Medicare before paying the treating practitioner, the fee charged is unsubstantiated. Co-payments for non-inpatient services (other than hospital substitute services, such as hospital-in-the-home services), count towards safety net thresholds, but only for substantiated services. Where a patient claims on Medicare before paying the treating practitioner, some practitioners subsequently accept a discounted fee for prompt payment.
- There is an anomaly in data capture for some bulk billed pathology claims, resulting in some apparent co-payments for these services. For all bulk billed services in recent years (and for the years examined in this study), the fee charged should equal the benefit paid.
- Total pathology services are included in total MBS services which greatly inflates the number of MBS services estimated.
- Data on MBS services exclude services to the Department of Veterans’ Affairs (DVA) card holders where care is reimbursed through DVA. It also excludes services by salaried GPs in residential aged care or outpatient departments. For more information on the use of DVA services by people living in residential aged care see: GP use by people living in permanent residential aged care, pages 7 and 8.
For the PBS/RPBS, this is because:
- data in the NIHSI AA exclude premiums paid by the patient, for example, brand or therapeutic premiums.
- From 1 January 2016, pharmacists have had the option of a $1 discount of the patient co-payment. The PBS/RPBS data in NIHSI AA do not reflect any such discounting.
- For under co-payment prescriptions, the patient contribution is an estimate reflecting the PBS value of the prescription and not the actual value paid at the pharmacy (which may have been discounted). Therefore, estimates from the PBS/RPBS may be overestimated.
- For under co-payment prescriptions, the NIHSI AA data do not include the ‘optional’ pharmacy fees of safety net recording fee and additional extra fee.
- Over-the-counter pharmaceuticals are not included.
Residential aged care services
Residential aged care services are not included in the health service use and cost estimates. Rather, health service use and costs for people who used residential aged care services (permanent residential and/or respite care) at any point in their last year of life are compared with those who did not use such care in their last year.
This analysis uses a flag to identify people who used residential aged care in their final year, not all of whom would have spent all 12 months in aged care or would have died in a residential aged care facility (some people living in aged care could have died elsewhere, such as in hospital) (AIHW 2021b).
There may be slightly different patterns of service use and associated costs if the length of time spent in residential aged care, as well as proximity to service use for people not in the last year of life, was factored into the analysis.
Community-based aged care, such as in-home palliative care and community nursing, are excluded.
Deaths
Deaths data used in this analysis are based on year of occurrence. These may differ from deaths data used in other AIHW publications that are based on year of registration.
Deaths where the underlying cause of death information was missing were excluded.
AIHW (Australian Institute of Health and Welfare) (2021a) National Mortality Database (NMD), aihw.gov.au, accessed
18 May 2022.
AIHW (2021b) Interfaces between aged care and health systems in Australia – where do older Australians die?, AIHW, Australian Government, accessed 17 February 2022.
Becker R, Silvi J, Ma Fat D, L’Hours A and Laurenti R (2006) A method for deriving leading causes of death. Bulletin of the World Health Organization 84:297–304.
Department of Health (2022) MBS Online Medicare Benefits Schedule, Department of Health website, accessed
29 June 2022.
| ABS | Australian Bureau of Statistics |
| ACT | Australian Capital Territory |
| AIHW | Australian Institute of Health and Welfare |
| ATC | Anatomical Therapeutic Chemical |
| COPD | chronic obstructive pulmonary disease |
| COVID-19 | coronavirus disease of 2019 |
| DVA | Department of Veterans Affairs |
| ED | emergency department |
| GPs | general practitioners |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, 10th Revision |
| MBS | Medicare Benefits Schedule |
| NDI | National Death Index |
| NEP | National Efficient Price |
| NIHSI AA | National Integrated Health Services Information Analysis Asset |
| NSW | New South Wales |
| NWAUs | National Weighted Activity Units |
| PBS | Pharmaceutical Benefits Scheme |
| RPBS | Repatriation Pharmaceutical Benefits Scheme |


