Mental health services
On this page:
What mental health services are available?
People with mental illness can access a variety of support services, which are funded and/or delivered by both the public and private sectors. Mental health care and support is provided across a range of settings and services, including:
- specialised hospital services – public and private
- specialised residential mental health services
- specialised community mental health care services
- primary care services.
Health care professionals who provide treatment, care and support within the mental health system include:
- general practitioners (GP)
- psychiatrists and other medical practitioners
- psychologists
- nurses
- social workers
- occupational therapists
- other allied health professionals
- mental health consumer and carer workers
- other personal care staff.
What do we know about mental illness?
Mental illness is a major health concern in Australia, with an estimated 43% of people aged 16–85 experiencing a mental disorder during their lifetime (ABS 2023). Systemically, Mental and substance use disorders have been responsible for around 15% of the total disease burden (AIHW 2023a). For more information, refer to Prevalence and impact of mental illness section.
Mental health services activity
Timely information on mental health systems is crucial in providing an early picture of activity across the system and meaningful comparisons to historical data. Service activity monitoring can provide insights into how the mental health system is delivering services and responding to changing population needs and events, such as the COVID-19 pandemic, natural disasters and policy changes. National services activity data are presented on this page for the December quarter 2023.
Medicare-subsidised mental health-specific services
Medicare-subsidised services are provided by psychiatrists, GPs, psychologists and other allied health professionals. They are delivered across a range of settings including hospitals, consulting rooms and at home (for example, home visits and telehealth).
Pharmaceutical Benefits Scheme prescriptions
The Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Benefits Scheme (RPBS) provide access to subsidised prescription medicines. For this report programs will be aggregated and reported as ‘PBS’.
In the December quarter 2023, over 12 million PBS-listed mental health-related medications were dispensed. This was 1% higher than the same quarter in 2022 and 3% higher than the same quarter in 2021.
National use of crisis and support organisations
Crisis and support organisations provide support to Australians experiencing mental health issues. There are a range of crisis, support and information services currently operating including Lifeline, Kids Helpline, Head to Health, ReachOut and Beyond Blue. National activity data for these organisations is reported here as contacts, representing service demand, and answered contacts, representing the total number of contacts answered by each organisation. Data for:
- Lifeline relate to phone calls
- Kids Helpline include phone, webchat and email contacts
- Beyond Blue include phone, webchat and email contacts
- Data from July 2020 to December 2022 includes contacts and answered contacts for both the Beyond Blue main service and dedicated COVID-19 service.
- ReachOut and Head to Health include the average number of website users per day, representing the average daily volume for website activity.
In the December quarter 2023, nationally there were about:
- 257,700 contacts made to Lifeline; per 100,000 population, this was 12% lower than the same quarter in 2022 and 14% lower than the same quarter in 2021
- 72,200 contacts made to Kids Helpline; per 100,000 population, this was 10% lower than the same quarter in 2022 and 16% lower than the same quarter in 2021
- 64,100 contacts made to Beyond Blue; per 100,000 population, this was 21% lower than the same quarter in 2022 and 18% lower than the same quarter in 2021
- 6,600 ReachOut website users per day (on average); per 100,000 population, this was 1% higher than the same quarter in 2022 and 17% higher than the same quarter in 2021
- 1,800 Head to Health website users per day (on average); per 100,000 population, this was 29% lower than the same quarter in 2022 and 1% lower than the same quarter in 2021.
Refer to the Mental health services activity monitoring: quarterly data page for further information on the activity data presented above, including data sources, a list of key events related to activity, and state and territory breakdowns.
Service use
Different types of services are accessed by people with a mental illness each year across the Australian health system. Selected annual findings from the Mental Health Online Report are summarised below (Table 1).
| Service type | Volume | Selected findings |
|---|---|---|
Medicare-subsidised mental health-related services(a) For more, refer to Medicare-subsidised services | Over 2.7 million patients accessed almost 13.2 million services in 2022–23 | Psychologists provided 49% of these services. 1 in 5 (22%) services were delivered via telehealth. More females (13%) accessed services compared to males (8%). |
Mental health-related prescriptions(b) For more, refer to Mental health prescriptions | 45.6 million prescriptions to 4.8 million patients in 2022–23 | 85% of prescriptions were through GPs. 73% of prescriptions were for antidepressant medication(b). |
Public sector community mental health care service contacts For more, refer to Community services | 9.6 million contacts by nearly 468,800 patients in 2021–22 | Aboriginal and Torres Strait Islander (First Nations) patients received community mental health care services at more than 3 times the rate of non-Indigenous patients. |
Public sector residential mental health care services For more, refer to Residential services | 9,000 episodes of residential care for 7,100 residents in 2021–22 | Schizophrenia was the most frequently reported principal diagnosis (22% of episodes). 16% of residents had an involuntary mental health legal status. 58% of episodes lasted 2 weeks or less. |
Emergency department (ED) services (public hospitals) For more, refer to Emergency departments | 287,500 presentations in 2022–23 | 75% were classified as urgent or semi-urgent. The most frequent diagnosis among ED presentation was Mental and behavioural disorders due to psychoactive substance use (27%). |
Psychosocial disability support services For more, refer to Psychosocial disability support | At 31 December 2021, 53,100 people with a primary psychosocial disability were NDIS active participants. | People with a psychosocial disability formed the third largest primary disability group among NDIS participants. The rate was almost 3 times higher for First Nations people than other Australians (468 and 164 per 100,000 respectively. |
Overnight admitted patient hospitalisations For more, refer to Admitted patients | 262,200 hospitalisations in 2021–22 | Schizophrenia (18%) and Depressive episode (12%) were the most common principal diagnoses for public hospitalisations with specialised psychiatric care. |
Same day admitted patient hospitalisations For more, refer to Admitted patients | 52,100 hospitalisations in 2021–22 | 25% of same day hospitalisations with specialised psychiatric care in public hospitals had a principal diagnosis of Depressive episode. |
| Specialist Homelessness Services (SHS) For more, refer to Specialist Homelessness Services | 31% of total SHS clients had a current mental health issue in 2022–23 | Main reason identified by clients for accessing services were housing crisis (21%), family and domestic violence (19%) private dwelling conditions (13%). |
- Includes psychiatrists, GPs, clinical psychologists, other psychologists and other allied health services. These services are billed as mental health-related items, which underestimates the total mental health-related activity, especially for services provided by GPs.
- Prescriptions subsidised and under co-payment under the Pharmaceutical Benefits Scheme and Repatriation Pharmaceutical Benefits Scheme.
Source: Mental Health (AIHW 2023b).
Spending
In real terms, about $12.2 billion, or $472 per capita, was spent on mental health-related services in Australia in 2021–22. $11.6 billion of this was government mental health expenditure, representing 7% of total government health expenditure. The total spending in 2021–22 in real terms included around $7.4 billion, or $286 per capita, spent on state and territory specialised services.
In current prices, in 2022–23 about $1.5 billion, or $58 per capita, was spent on Medicare-subsidised services and $635 million, or $26 per capita, was spent on PBS prescriptions.
For more information, refer to Expenditure on mental health-related services.
Workforce
A variety of professions deliver care and support to people with mental illness, including psychologists, psychiatrists, mental health nurses, occupational therapists, social workers, GPs, counsellors and peer workers. Available data for some of these professions indicate that in Australia in 2021 there were about:
- 31,400 psychologists
- 4,000 psychiatrists
- 25,000 mental health nurses
- 2,600 mental health occupational therapists
- 2,600 accredited mental health social workers.
For more information, refer to Mental health workforce.
Facilities
While professionals work across a range of settings, some work in specialised mental health care facilities. These specialised mental health care facilities are a key component in delivering mental health care in Australia. In 2021–22, there were about 37,000 full-time equivalent staff employed in state and territory specialised mental health care services.
For more information, refer to Specialised mental health care facilities.
Safety and quality
Safety and quality are important in all areas of the health system. Data are available that can be used to measure aspects of safety and quality in the Australian mental health care system, including:
- use of restrictive practices
- consumer perspectives of care
- change in mental health consumers’ clinical outcomes.
Seclusion and restraint
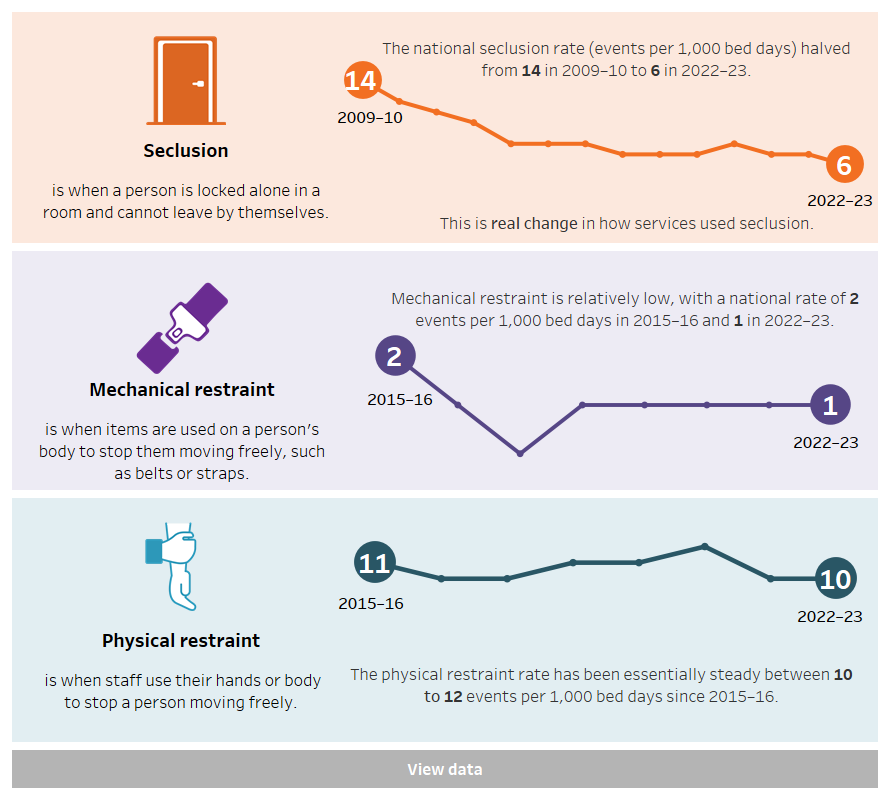
Seclusion is defined as the confinement of a patient alone in a room or area from which free exit is prevented. Restraint is defined as the restriction of an individual's freedom of movement by physical or mechanical means.
Reducing, and where possible, eliminating the use of seclusion and restraint is a policy priority in Australian mental health care and has been supported by changes to legislation, policy and clinical practice (RANZCP 2021).
Seclusion events in specialised acute public hospital mental health services have more than halved from 14 seclusion events per 1,000 bed days in 2009–10 to 6 events in 2022–23 (Figure 1).
Mechanical restraint events have remained at 1 event per 1,000 bed days of patient care since 2018–19. The use of physical restraint has remained relatively stable since 2015–16, varying between 10 to 12 events per 1,000 bed days of patient care (Figure 1).
Figure 1: Seclusion and restraint in Australia public sector acute mental health hospital services, 2009–10 to 2022–23
Three line graphs showing seclusion rate (events per 1,000 bed days) in Australia from 2009–10 to 2022–23 and mechanical and physical restraint rate from 2015–16 to 2022–23. The national seclusion rate more than halved from 2009–10 (14) to 2022–23 (6).. Mechanical restraint has remained consistently low from 2 events per 1,000 beds days in 2015–16 to 1 since 2018–19. The physical restraint rate has stayed consistent at 11 events per 1,000 bed days in 2015–16 to 12 events in 2022–23.
Source: National Seclusion and Restraint Database, Tables SECREST.1 and 4.
For more information refer to Seclusion and restraint.
Involuntary treatment
Involuntary treatment is compulsory assessment or treatment of people in mental health services without the person’s consent being given. This is a restrictive practice and can be legally approved under certain conditions.
Involuntary treatment is used in Australian mental health services for about:
- 15% of community care contacts
- 16% of residential care episodes
- 45% of hospitalisations in acute units
- 29% of hospitalisations in non-acute units.
For more information refer to Involuntary treatment in mental health care.
Patient-reported experiences of care
Measures of patient-reported experience collect patients’ views and observations on aspects of the care they have received. One such measure – the Your Experience of Service (YES) survey – has been implemented in New South Wales, Victoria and Queensland specialised mental health services. Each state has a method of administration that best suits local needs and, therefore, comparisons between jurisdictions with different methods should be made with caution.
In 2021–22, more than 24,500 YES survey responses were collected from 86 mental health service organisations across New South Wales, Victoria and Queensland.
It is estimated that:
- 69% of respondents in New South Wales, 51% in Victoria and 47% in Queensland reported a positive experience of admitted care services
- 78% of respondents in New South Wales, 70% in Victoria and 80% in Queensland reported a positive experience of ambulatory (non-admitted) care services
- 80% of respondents in Victoria and 77% in Queensland residential care reported a positive experience of service.
For more information refer to Consumer perspectives of mental health care.
Consumer outcomes of care
Clinical measures that capture information about the health and wellbeing of people during mental health service use can be used to report on whether consumers improve after receiving care. The National Outcomes and Casemix Collection includes data on outcome measures from all publicly funded or managed mental health services. In 2021–22, information for more than 200,000 people was recorded, representing 42% of consumers of public mental health services.
In 2021–22, clinician-rated measures showed Improvement outcomes for patients in:
- admitted (inpatient) care, at 58% (aged 11–17), 72% (aged 18–64) and 73% (65 and older) of episodes.
- ambulatory (non-admitted) care, at 54% (aged 11–17), 50% (aged 18–64), and 47% (65 and older) of episodes.
For more information refer to Consumer outcomes in mental health care.
Performance indicators
A key performance indicator (KPI) is a measure that describes a situation concisely, helps track progress and performance and acts as a guide to inform decision making. In the public mental health sector, these indicators cover different aspects of services. They can inform consumers', service providers' and funders' impressions of service and service performance.
For more information on the latest Key Performance Indicators for Australian Public Mental Health Services and National Healthcare Agreement Indicators, refer to Mental health performance indicators.
Where can I find more information?
For more information on mental health services refer to:
If you or someone you know needs help please call:
| Key concept | Description |
|---|---|
| Admitted care: | A specialised mental health service that provides overnight care in a psychiatric hospital or a specialised mental health unit in an acute hospital. Psychiatric hospitals and specialised mental health units in acute hospitals are establishments devoted primarily to the treatment and care of admitted patients with psychiatric, mental or behavioural disorders. These services are staffed by health professionals with specialist mental health qualifications or training and have as their principal function the treatment and care of patients affected by mental disorder/illness. |
| Admitted patient: | A patient who undergoes a hospital's formal admission process. |
| Ambulatory care: | A specialised mental health service that provides services to people who are not currently admitted to a mental health admitted or residential service. Services are delivered by health professionals with specialist mental health qualifications or training. Ambulatory mental health services include:
|
| Burden of disease and injury: | A term referring to the quantified impact of a disease or injury on an individual or population, using the disability-adjusted life year (DALY) measure. |
| Hospitalisation: | Synonymous with admission and separation; that is, an episode of hospital care that starts with the formal admission process and ends with the formal separation process. An episode of care can be completed by the patient’s being discharged, being transferred to another hospital or care facility, or dying, or by a portion of a hospital stay starting or ending in a change of type of care (for example, from acute to rehabilitation). |
| Mental health-related medications: | Benefit-paid pharmaceuticals and other medications defined in this section as 5 selected medication groups as classified in the Anatomical Therapeutic Chemical (ATC) Classification System (WHO 2022), namely antipsychotics (code N05A), anxiolytics (code N05B), hypnotics and sedatives (code N05C), antidepressants (code N06A), and psychostimulants, agents used for ADHD and nootropics (code N06B) – prescribed by all medical practitioners (that is, general practitioners (GPs), non‑psychiatrist specialists and psychiatrists). Data include PBS-subsidised (above-co-payment) and under-co-payment prescriptions. More information can be found in the Mental health-related prescriptions section of the Mental Health Online Report. |
| Restraint: | The restriction of an individual's freedom of movement by physical or mechanical means. The application of devices (including belts, harnesses, manacles, sheets and straps) on a person's body to restrict his or her movement. This is to prevent the person from harming himself/herself or endangering others or to ensure the provision of essential medical treatment. It does not include the use of furniture (including beds with cot sides and chairs with tables fitted on their arms) that restricts the person's capacity to get off the furniture except where the devices are used solely for the purpose of restraining a person's freedom of movement. The use of a medical or surgical appliance for the proper treatment of physical disorder or injury is not considered mechanical restraint. The application by health care staff of ‘hands-on’ immobilisation or the physical restriction of a person to prevent the person from harming himself/herself or endangering others or to ensure the provision of essential medical treatment. |
| Seclusion: | The confinement of the consumer at any time of the day or night alone in a room or area from which free exit is prevented. Key elements include that:
The intended purpose of the confinement is not relevant in determining what is or is not seclusion. Seclusion applies even if the consumer agrees or requests the confinement. The awareness of the consumer that they are confined alone and denied exit is not relevant in determining what is or is not seclusion. The structure and dimensions of the area to which the consumer is confined is not relevant in determining what is or is not seclusion. The area may be an open area, for example, a courtyard. Seclusion does not include confinement of consumers to High Dependency sections of gazetted mental health units, unless it meets the definition. |
| Service contact (community mental health care) | The provision of a clinically significant service by a specialised mental health service provider for patient/clients, other than those admitted to psychiatric hospitals or designated psychiatric units in acute care hospitals and those resident in 24‑hour staffed specialised residential mental health services, where the nature of the service would normally warrant a dated entry in the clinical record of the patient/client in question. Any one patient can have one or more service contacts over the relevant financial year period. Service contacts are not restricted to face‑to‑face communication but can include telephone, video link or other forms of direct communication. Service contacts can also be either with the patient or with a third party, such as a carer or family member, and/or other professional or mental health worker, or other service provider. |
| Specialised mental health care facilities | Specialised facilities that deliver and provide support for mental health care. These can include public and private psychiatric hospitals, psychiatric units or wards in public acute hospitals, Community mental health care services and government-operated and non-government-operated Residential mental health services. More information can be found in Specialised mental health care facilities. |
ABS (Australian Bureau of Statistics) (2023) National Study of Mental Health and Wellbeing, ABS, accessed 17 January 2024.
AIHW (Australian Institute of Health and Welfare) (2023) Australian Burden of Disease Study 2023: Burden of disease in Australia, AIHW website, accessed 17 January 2024.
AIHW (2024) Mental health: Topic areas summary, AIHW website, accessed 17 January 2024.
RANZCP (Royal Australian and New Zealand College of Psychiatrists) (2021) Position Statement 61: Minimising and, where possible, eliminating the use of seclusion and restraint in people with mental illness, RANZCP website, accessed 17 January 2024.
WHO (World Health Organisation) (2022), ATC: Structure and principles, Oslo: WHO Collaborating Centre for Drug Statistics Methodology, accessed 17 January 2024.
This section was last updated on 30 April 2024.


