Palliative care in general practice
General practitioners (GPs) play an important role in palliative care as well as the health-care system more broadly. However, there is no nationally consistent, routinely collected primary healthcare data collection that enables reporting on the provision of palliative care by GPs.
Furthermore, while the Medicare Benefits Schedule (MBS) includes specific items for palliative medicine specialist services (delivered by palliative medicine specialists) for which it will reimburse a proportion of the MBS fee (see Services provided by palliative medicine specialists section) there are no palliative care-specific items that can be used by GPs or other medical specialists who may be providing palliative care (such as oncologists). It is therefore likely that GPs use other MBS items, for example, those for chronic disease management and home visit items, when providing patients with palliative care. Consequently, the extent of palliative care-related services delivered by GPs cannot be established from existing Medicare data.
This section presents information on palliative care-related encounters provided by GPs using data from the Bettering the Evaluation and Care of Health (BEACH) survey of general practice activity. The BEACH survey was run for the last time in 2015–16.
Downloads
The information in this section was last updated in October 2017.
Key points
- In 2015–16, about 1 in 1,000 GP encounters reported for the BEACH collection was palliative care-related.
- About 9 in 10 palliative care encounters were with people aged 65 and over, and 4.8% were with those aged under 55.
- Females accounted for a greater proportion of GP palliative care-related encounters (53.0%) than males (47.0%), but there was no difference between the sexes in palliative care encounter rates (about 1 per 1,000 of GP encounters for both males and females).
- In 2015–16, 1.3% of palliative care-related encounters were recorded as being with Indigenous Australians.
BEACH survey data
The BEACH survey is a paper-based survey of a sample of GPs and their encounters with patients. The BEACH survey provides information on the reasons patients visited the GP, the problems managed and the types of management provided for each problem.
The 2015–16 BEACH data presented in this section relate to 96,500 GP encounters from a sample of 965 GPs over the period from April 2015 to March 2016, inclusive. After weighting (to ensure that national general practitioner age, sex and activity patterns are reflected) the data include 97,398 (weighted) encounters (Britt et al. 2016). For further information about the 2015–16 BEACH survey methodology see the Family Medicine Research Centre General practice activity in Australia 2015–16 report.
Palliative care-related encounters in this section have been identified using the 4 ICPC-2 PLUS palliative care-related codes that were recorded against three discrete BEACH survey data elements (Reason for encounter, Problem/Diagnosis and Referral).
More information about this survey and the data is in the Technical information section.
Palliative care-related encounters
According to BEACH, about 1 in 1,000 GP encounters in 2015–16 were palliative care-related. This corresponds to approximately 6 encounters per 1,000 population in 2015–16. It should be noted that palliative care-related GP encounters are difficult to define as palliative care is not a medical diagnosis in its own right; rather, it is a process related to a stage in managing an illness. As such, GPs may record the problems they manage as part of the palliative care process (for example, lung cancer)—not the palliative care process itself. In cases where the patient’s health is gradually deteriorating and there is no specific problem being dealt with, palliative care may be recorded as the problem managed. As such, the number of encounters reported as palliative care is likely to be an underestimate of the actual number of palliative care-related encounters by GPs.
Patient demographics
In 2015–16, about 9 in 10 palliative care GP encounters were with people aged 65 and over, and 4.8% with those aged under 55 (Figure GP.1). Females accounted for a greater proportion of GP palliative care-related encounters (53.0%) than males (47.0%), but there was no difference between the sexes in palliative care encounter rates (about 1 per 1,000 of encounters with both males and females). In 2015–16, 1.3% of palliative care-related encounters were recorded as being with Indigenous Australians, less than half the proportion of the general population which is Indigenous.
Figure GP.1: Palliative care-related GP encounters by age group, 2015–16
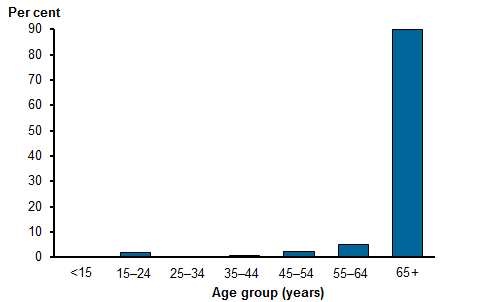
Source data: Family Medicine Research Centre (University of Sydney) 2017 analysis of BEACH Survey 2015–16
Source: Palliative care in general practice tables 2015-16.
General practice palliative care-related attitudes and awareness
A study commissioned by the Australian Government Department of Health researching the awareness, attitudes and provision of best practice advance care planning, palliative care and end of life care within general practice estimated that palliative care consultations account for about 1 in every 100 GP consultations (1%) (Department of Health 2017). The differences in the results between this survey and the BEACH survey are likely to be due to different methodologies including aspects such as the composition of the populations of GPs who responded to each survey and how a palliative care encounter or consultation was defined.
Other findings from this survey were that GPs’ understanding of what constitutes palliative care and end of life care varies widely and that differing palliative care settings have very different requirements in terms of best practice. The report on the survey also provided a range of recommendations including better defining the role of GPs in palliative care, promoting a better understanding of the clinical triggers for commencing palliative care, the development of local directories to enable GPs to access palliative care resources and better communication and integration with other parts of the health system including encouraging referrals to specialist palliative care teams or GP experts (Department of Health 2017).
The discontinuation of the BEACH survey (which ran from 1998 to 2016) presents a challenge for future reporting on the pivotal role that general practitioners have in delivering high quality palliative care. AIHW is currently working with stakeholders to establish a consistent data collection on palliative care activity in general practice, to better inform the community and enable decision-makers at all levels to monitor GPs’ provision of high quality palliative care to Australians that meets their needs.
References
Britt H, Miller GC, Henderson J, Bayram C, Harrison C, Valenti L et al. 2016. General practice activity in Australia 2015–16. General practice series no. 40. Sydney: Sydney University Press.
DOH (Department of Health) 2017. Final report: research into awareness, attitudes and provision of best practice advance care planning, palliative care and end of life care within general practice. Canberra: Department of Health.


