Overarching methods and choices for risk factors
On this page:
A risk factor is any determinant that causes (or increases the likelihood of) one or more diseases or injuries. As well as providing estimates of fatal and non-fatal burden, burden of disease methodology allows death and health loss to be attributed to specific underlying (or linked) risk factors. Quantification of the impact of risk factors assists evidence-based decisions about where to direct efforts to prevent disease and injury and to improve population health.
The methods used to quantify the impact of risk factors in the ABDS 2018 are described in this chapter (see specific risk factor methods for detail on each risk factor).
Box 2.3: Key terms used in this chapter
attributable burden: The disease burden attributed to a particular risk factor. It is the reduction in burden that would have occurred if exposure to the risk factor had been avoided or had been reduced to its theoretical minimum risk exposure distribution (TMRED).
counterfactual: An alternative risk factor exposure distribution chosen for comparison with the observed distribution, to estimate the alterable contribution of that risk factor to the burden of disease. The most commonly used counterfactual in burden of disease studies is the theoretical minimum risk exposure distribution (TMRED).
effect modification: A change in the observed magnitude or direction of an association between a risk exposure and an outcome when a third variable (such as age or sex) is included in the analysis.
effect size: A statistical measure of the strength of the relationship between 2 variables (in this context, between a risk exposure and a disease outcome), expressed, for example, as a relative risk or odds ratio.
linked disease: A disease or injury for which there is evidence that its likelihood is increased by the risk factor in question.
population attributable fraction (PAF): For a particular risk factor and causally linked disease or injury, the percentage reduction in burden that would occur for a population if exposure to the risk factor was avoided or reduced to its theoretical minimum.
relative risk (RR): The risk of an event relative to exposure, calculated as the ratio of the probability of the event’s occurring in the exposed group to the probability of its occurring in the unexposed group.
risk exposure distribution: The measure of the spread or distribution of exposure to the risk factor in the population that have encountered or experienced, or have the risk factor.
risk factor: Any factor that causes or increases the likelihood of illness or death due to a disease or injury or other unwanted condition or event.
theoretical minimum risk exposure distribution (TMRED): The risk factor exposure distribution that will lead to the lowest conceivable disease burden
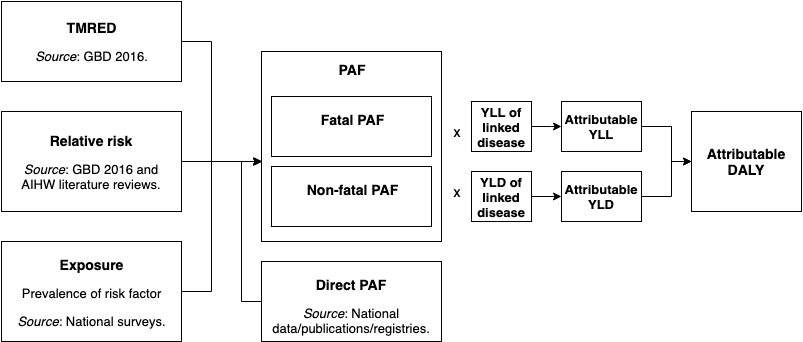
The burden attributable to risk factors is generally estimated using PAFs applied to the disease burden estimated as described in the disease burden sections.
Methodological developments in the ABDS 2018
Most of the risk factors methods were the same as those used in the ABDS 2015. However, some methods have changed following new risk factor methods by GBD 2019 and expert advice (GBD 2019 Risk Factors Collaborators 2020).
The most notable of these was the changes to physical inactivity and the dietary risk factors which both had changes to the categories of exposure that increased risk and the minimum exposure associated with increased risk (TMRED). These changes are described in detail in Risk factor specific methods section, a summary of the major changes are outlined below.
The methods for the dietary risk factor Diet high in sugar sweetened beverages changed to be directly linked to type 2 diabetes and coronary heart disease instead of mediating through overweight (including obesity).
Exposure to air pollution was also estimated from satellites calibrated with ground monitoring stations, instead of ground monitoring stations alone, improving the coverage of estimates for Australia.
Two new risk factors have been included: bullying victimisation and low birthweight & short gestation. Both risk factors were included in GBD 2019; however, the methods used in ABDS 2018 for bullying victimisation were based on Australian specific studies (Jadambaa 2019a, Jadambaa 2019b).
Steps in estimating risk factor attributable burden
The basic steps of estimating risk factor attributable burden are:
- select risk factors
- identify linked diseases based on convincing or probable evidence in the literature that the risk factor has a causal association with increased prevalence or mortality
- define the exposure to the risk factor that is not associated with increased risk of disease (the theoretical minimum risk exposure distribution, or TMRED, or counterfactual)
- estimate the PAFs by either a direct method or the comparative risk assessment method:
- if PAFs appropriate to the disease and population in question are available from a comprehensive data source (such as a disease register), they are estimated directly from this data source (named a direct PAF in this report) and do not require steps 5, 6 and 7
- if not, PAFs are created using the comparative risk assessment method, which involves steps 5, 6 and 7
- define the amount of increased risk (relative risk) of morbidity or mortality for the linked disease due to exposure to the risk factor
- estimate exposure to each risk factor in the population
- use these inputs to calculate the PAF. The PAF has a value between 0 and 1, where 0 means there was no burden attributable to the risk factor and 1 means that all the burden for the linked disease was attributable to the risk factor.
The burden attributable to each risk factor is calculated by applying the PAFs for each linked disease to the relevant YLL and YLD.
This process is shown in the figure below.
Figure 2.2: Inputs and processes to calculate attributable burden
Selection of risk factors
The risk factor list describes the specific risk factors considered as underlying causes of health loss through their causal association with particular diseases. In contrast to the disease list, which is exhaustive, and where an established classification system (the International Statistical Classification of Diseases and Related Health Problems) exists, the list of potential risk factors is near limitless, and there is often no consensus in the literature on what level(s) of exposure constitute ‘risk’. A predetermined set of criteria was used to develop the list, taking into account the potential for modification of exposure in the population, the availability of data on exposure, and the quality of evidence about the presence and magnitude of causal effects.
To be included in the ABDS 2018, a risk factor had to satisfy one or more of the following criteria:
Included in other studies’ risk factor lists
- Have been included in:
- the GBD 2019
- the ABDS 2011 or ABDS 2015 unless its inclusion in the ABDS 2018 conflicted with other criteria.
Substantial impact and policy interest
- Be of considerable importance to national or Indigenous disease burden based on previous studies (ABDS 2011, ABDS 2015; GBD 2019).
- Be of substantial Australian or Indigenous health policy interest – defined as currently being the focus of policy concern, professional attention or monitoring activity.
- Be modifiable, and able to be prevented or modified through policy intervention.
Be able to be measured
- Be measurable, including having:
- sufficient evidence for causal association between exposure and health outcomes based on high-quality epidemiological studies
- enough data and methods to enable exposure distributions to be estimated
- enough data to estimate effect sizes per unit of exposure of outcome-specific impacts
- evidence to support the ability of effect sizes to be generalised to populations, other than those included in the available studies, or to satisfactory models for extrapolating them.
ABDS 2018 risk factor list
The ABDS 2018 identified 40 risk factor components or exposures (such as cannabis and cocaine use) that combine to 20 individual risk factors (such as illicit drug use). These were broadly grouped into categories (behavioural, metabolic/biomedical and environmental risks).
|
Behavioural |
|
|---|---|
|
Environmental |
|
|
Metabolic/ Biomedical |
|
Due to methodological reasons, many of these 20 risk factors are the sum of estimates from different measures of exposure to risk factors that are in addition to the 40 reported (for example, tobacco use is the sum of current tobacco use and the smoking impact ratio). These measures of exposure are listed for each risk factor in Estimating attribution to risk factors.
There is a high and complex degree of interrelatedness between the chosen risk factors, potentially causing biases. For this reason, risk factors were analysed and reported individually. A combined estimate is reported for all risk factors and for all dietary risk factors – using a multiplicative method that adjusts for the co-occurrence of multiple risk factors – to estimate the burden attributable to multiple risk factors (described in the section headed Combined risk factor analysis).
Risk factors not included in the ABDS 2018
Sub-optimal breastfeeding and exposure to lead (included in the GBD) were not included in the ABDS 2018 as sub-optimal breastfeeding was linked in the global studies to intestinal infection diseases that are not common in Australia. Exposure to lead was also excluded because exposure data (estimates of bone lead levels) were not available for Australia.
Social determinants of health (the economic and social conditions – such as income, level of education and employment status – that influence health status) could not be included as risk factors in the current study. This was due to the resources that would have been needed to undertake the large and complex body of work required (such as developing appropriate definitions directly related to health, and sourcing disease-specific relative risks). Estimating exposure to social determinants is further complicated in that their impact can be accumulative over the life course and subsequent generations (Atkinson et al. 2010; Zubrick et al. 2010). The AIHW recognises this as an important area of work for future burden of disease studies. Some indication of the effect of social determinants on the health burden is provided by estimating burden by socioeconomic area in this study.
Work was begun as part of this study to estimate the contribution of heatwaves to the burden of disease. This risk factor was found to meet the criteria for inclusion but further methodological and data developments are needed before it can be included.
Selection of linked diseases
A linked disease is a condition in the disease list with a known risk factor for that condition. For example, high blood plasma glucose is a risk factor for diabetes, coronary heart disease, cerebrovascular disease and chronic kidney disease. In this report, such associations are described as diseases or injuries being ‘linked to’ that risk factor. Thus, these diseases are linked to the risk factor high blood plasma glucose. The risk factors and linked diseases selected for the ABDS 2018 risk factors are shown in risk factor specific methods.
Linked diseases were included where there was sufficient evidence of a causal link. This is defined as having convincing or probable evidence measured against criteria based on World Health Organization modifications to the World Cancer Research Fund grading system:
- Convincing evidence – evidence based on epidemiological studies showing consistent associations between exposure and disease, with little or no evidence to the contrary. The available evidence is based on a substantial number of studies, including prospective observational studies and, where relevant, randomised controlled trials of sufficient size, duration and quality, showing consistent effects. The association should be biologically plausible.
- Probable evidence – evidence based on epidemiological studies showing fairly consistent associations between exposure and disease, but for which there are perceived shortcomings in the available evidence, or some evidence to the contrary, which preclude a more definite judgement. Shortcomings in this evidence might be any of the following insufficient duration of trials (or studies), insufficient trials (or studies) available, inadequate sample sizes, or incomplete follow-up. Laboratory evidence is usually supportive. The association should be biologically plausible.
- Possible evidence – evidence based mainly on findings from case-control and cross‑sectional studies. Insufficient randomised controlled trials, observational studies, or non-randomised controlled trials are available. Evidence based on non‑epidemiological studies, such as clinical or laboratory investigations, is supportive. More trials are needed to support the tentative associations, which should be biologically plausible.
- Insufficient evidence – evidence based on findings of a few studies that are suggestive, but insufficient to establish an association between exposure and disease. Little or no evidence is available from randomised controlled trials. More well-designed research is needed to support the tentative association.
The linked diseases were spread across 15 disease groups. Some risk factors had a single linked disease, while others were paired with many outcomes across the disease groups.
The ABDS 2018 adopted relevant linked diseases used in the GBD 2019 (GBD 2019 Risk Factors Collaborators 2020) and those identified by the AIHW from literature reviews for selected risk factors as part of extension projects (AIHW 2016a, 2017a, 2017b, 2018). The details of why any additional linked diseases were selected or not included when compared with the GBD is described in the methods chapter of these reports.
The linked diseases for dietary risk factors were reviewed as part of this study, based on the GBD 2019, a literature review and expert advice. The risk factor diet high in sodium was linked to other risk factors (high blood pressure), which then linked to diseases. The impact was estimated by the amount sodium consumption influences blood pressure and therefore the diseases linked to high blood pressure.
Dementia was linked to risk factors where it was identified by the AIHW as having sufficient evidence (risk factor specific methods, AIHW 2016b).
Additional material
National and Indigenous-specific data sources were used to compile risk factor exposure distributions. Survey and administrative data sets were primary sources of exposure data. In the absence of good-quality survey or administrative data, epidemiological studies were used to determine exposures distributions. Administrative data sources were evaluated for their level of ascertainment and coverage. Surveys were evaluated for their representativeness, potential selection bias and measurement bias (validity and reliability of measurement). Epidemiological studies were assessed for the quality of their study design, their timeliness, credibility, representativeness, and sources of bias or error.
Potential sources of data needed to have had comparable exposure definition; be relevant to the Australian population; and be timely, accurate, reliable and credible.
Published and unpublished data sources were assessed according to the criteria in Box 2.4. These criteria are largely based on the ABS’s Data Quality Framework, but have been modified in some areas to better suit the range of data sources used for burden of disease analyses, including epidemiological studies.
Not all of the criteria were applicable to all types of data sources assessed, and not all dimensions were weighted equally as the importance of each dimension depends on the type of data source.
Box 2.4: Criteria for risk factor exposure data selection
Comparability
The data source should use an exposure definition that is comparable with that used for both the effect size and the counterfactual distribution. This definition is decided on a case-by-case basis for each risk factor on the risk factor list. The 3 options of comparability are:
- consistent if the exposure definition is the same as the reference definition
- comparable if the exposure definitions can be aligned
- inconsistent if the exposure definitions are different and cannot be aligned.
Relevance and representativeness
Exposure distributions should ideally be drawn from Australian studies. If these are not available, they may be sourced from populations comparable with the Australian population. Care will need to be taken to ensure data are representative of both the Indigenous and non-Indigenous population. The 3 options of relevance for national estimates are:
- Australian population (national)
- Australian population (sub-national)
- regional population (such as New Zealand, the United States of America, Canada).
Currency
The data source should ideally be within 5 years of the reference year. Data sources for 2003–2009 may also be included if no later data sources are available.
Accuracy
The data source should ideally have more than 90% case ascertainment or coverage of the population of interest, and a RSE or CI of less than 25%.
The 3 options for ascertainment/coverage are:
- more than 90% ascertainment or coverage
- 60%–90% ascertainment or coverage
- below 60% ascertainment or coverage.
The 3 options for sources of error (sampling/non-sampling) are:
- RSE or CI width of less than 25% of the estimate
- RSE or CI width of 25%–50% of the estimate
- RSE or CI width greater than 50% of the estimate.
Measurement error
Data surrounding physiological and biomedical risk factors should ideally be collected and reported by clinical tests, or using similar tests in a survey setting. Self-reported data may be used but will need to be assessed for validity. The 2 options for measurement error are:
- clinically reported or measurement data
- self-reported.
Validation
The data source should have been validated. In the case of surveys, the questionnaire should have been validated against a gold standard measurement. In the case of administrative data, the data should have been validated by the agency or organisation that manages the data collection. In the case of epidemiological studies, the results should have been validated against results from other studies to determine whether they are plausible. The 2 options for validation are:
- validated
- not validated.
Credibility
The data source should be collected and/or managed by a credible institution, such as a national or state/territory statistical agency or a recognised university or research organisation. For epidemiological studies, ideally, estimates from the data source will have been published and peer-reviewed. The 4 options for credibility of the estimates are:
- published and peer reviewed
- published but not peer reviewed
- not published but peer reviewed
- not published and not peer reviewed.
Accessibility/timeliness
The data source at the required level of disaggregation must be available to the AIHW with sufficient time for analysis. This criterion will identify issues of accessibility, and help to prioritise data sources where such issues exist. The 3 options for availability of data are:
- currently available
- available with enough time for burden of disease analysis
- unlikely to be available with enough time for burden of disease analysis.
Each data source was scored against the assessment matrix below.
- Any data source scoring predominantly high was included in the ABDS, provided that:
- components of comparability, relevance/representativeness, currency, and accuracy (ascertainment/coverage) were high or medium for administrative data
- components of comparability, relevance/representativeness, currency, and accuracy (non-random error) were scored high or medium for survey data
- components of comparability, relevance/representativeness, currency, and credibility were scored high or medium for epidemiological studies.
- A data source scoring predominantly medium was used if no other data sources for the relevant condition existed, or if there were issues with availability of better data.
-
A data source scoring predominantly low was not included.
| Rating | High | Medium | Low |
|---|---|---|---|
|
Comparability |
Consistent |
Comparable |
Inconsistent |
|
Relevance – National study |
National |
Sub-national |
Sub- or super-regional |
|
Relevance – Indigenous study |
Indigenous |
Sub-national or Total Australian or non‑Indigenous |
Other Indigenous population (New Zealand, United States, Canada) |
|
Currency |
2013 or later |
2007–2013 |
Before 2007 |
|
Accuracy – coverage |
More than 90% |
60%–90% |
Less than 60% |
|
Accuracy – sampling |
Less than 25% RSE |
25%–50% RSE |
More than 50% RSE |
|
Accuracy – measurement |
Clinically reported or measured |
Self-reported |
Not known |
|
Validation |
Validated |
Validated or not validated |
Not validated |
|
Credibility |
Published and Peer reviewed |
Published but not peer reviewed or not published but peer reviewed |
Not published nor peer reviewed |
|
Accessibility/ timeliness |
Currently available |
Expected to be available in time for analysis |
Unlikely to be available in time for analysis. |
AIHW 2016a. Diabetes and chronic kidney disease as risks for other diseases. Australian Burden of Disease Study 2011. Australian Burden of Disease Study series no. 8. Cat. no. BOD 9. Canberra: AIHW.
AIHW 2016b. Contribution of vascular diseases and risk factors to the burden of dementia in Australia: Australian Burden of Disease Study 2011. Australian Burden of Disease Study series no. 9. Cat. no. BOD 10. Canberra: AIHW.
AIHW 2017a. Impact of physical inactivity as a risk factor for chronic conditions: Australian Burden of Disease Study. Australian Burden of Disease Study series no. 15. Cat. no. BOD 16. Canberra: AIHW.
AIHW 2017b. Impact of overweight and obesity as a risk factor for chronic conditions: Australian Burden of Disease Study. Australian Burden of Disease Study series no. 11. Cat. no. BOD 12. Canberra: AIHW.
AIHW 2018. Impact of alcohol and illicit drug use on the burden of disease and injury in Australia: Australian Burden of Disease Study 2011. Australian Burden of Disease Study series no. 17. Cat. no. BOD 19. Canberra: AIHW.
Atkinson J, Nelson J & Atkinson C 2010. Trauma, transgenerational transfer and effects of community wellbeing. In Purdie N, Dudgeon P & Walker R (eds). Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. Canberra: Department of Health and Ageing: 135–44.
GBD 2019 Risk Factors Collaborators 2020. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396:1223–249.
Jadambaa A, Thomas HJ, Scott JG, Graves N, Brain D & Pacella R 2019a. Prevalence of traditional bullying and cyberbullying among children and adolescents in Australia: A systematic review and meta-analysis. Australian & New Zealand Journal of Psychiatry 53:878–888.
Jadambaa A, Thomas HJ, Scott JG, Graves N, Brain D & Pacella R 2019b. The contribution of bullying victimisation to the burden of anxiety and depressive disorders in Australia. Epidemiology and Psychiatric Sciences 29:1–23.
Zubrick SR, Dudgeon P, Gee G, Glaskin B, Kelly K, Paradies Y et al. 2010. Social determinants of Aboriginal and Torres Strait Islander social and emotional wellbeing. In Purdie N, Dudgeon P & Walker R (eds). Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. Canberra: Department of Health and Ageing.


