Physical health of people with mental illness
Citation
AIHW
Australian Institute of Health and Welfare (2024) Physical health of people with mental illness, AIHW, Australian Government, accessed 28 April 2024.
APA
Australian Institute of Health and Welfare. (2024). Physical health of people with mental illness. Retrieved from https://pp.aihw.gov.au/reports/mental-health/physical-health-of-people-with-mental-illness
MLA
Physical health of people with mental illness. Australian Institute of Health and Welfare, 14 February 2024, https://pp.aihw.gov.au/reports/mental-health/physical-health-of-people-with-mental-illness
Vancouver
Australian Institute of Health and Welfare. Physical health of people with mental illness [Internet]. Canberra: Australian Institute of Health and Welfare, 2024 [cited 2024 Apr. 28]. Available from: https://pp.aihw.gov.au/reports/mental-health/physical-health-of-people-with-mental-illness
Harvard
Australian Institute of Health and Welfare (AIHW) 2024, Physical health of people with mental illness, viewed 28 April 2024, https://pp.aihw.gov.au/reports/mental-health/physical-health-of-people-with-mental-illness
Get citations as an Endnote file: Endnote
On this page:
Key points
People living with mental illness are more likely to experience poorer physical health than the general population.

People living with mental illness, and especially severe mental illness, tend to die earlier than the general population.

Almost 80% of premature deaths of people with mental illness are due to preventable physical health conditions.
People living with mental illness, and in particular severe mental illness (SMI), are more likely to experience comorbidity of physical conditions, more likely to be hospitalised for potentially preventable reasons and tend to die earlier than the general population (Sara et al. 2021; Lawrence et al. 2013).
For more information on mental illness, see the Mental Health Online Report.
Reporting on the physical health of people with mental illness
There is information on the prevalence of physical illness among people living with mental illness from population-based data sources, such as the National Study of Mental Health and Wellbeing (NSMHW), National Health Survey (NHS) and the Census of Population and Housing. One challenge in reporting on the physical health of people experiencing mental illness is a lack of consistent health systems data. Initiatives and programs that monitor the physical heath of Australians with mental illness may provide insight, but they are not consistent across jurisdictions and different health settings.
How common is physical illness among people with mental illness?
According to the 2020–2022 NSMHW, an estimated 4.3 million Australians aged 16–85 years, or 22% of this population, had experienced a mental disorder in the 12 months prior to the study. Of these, 2 in 5 (39%) also had a long-term physical health condition. This represents an estimated 1.7 million people or 1 in 12 (8.4%) adults experiencing both a mental illness and a long-term physical health condition (ABS 2023).
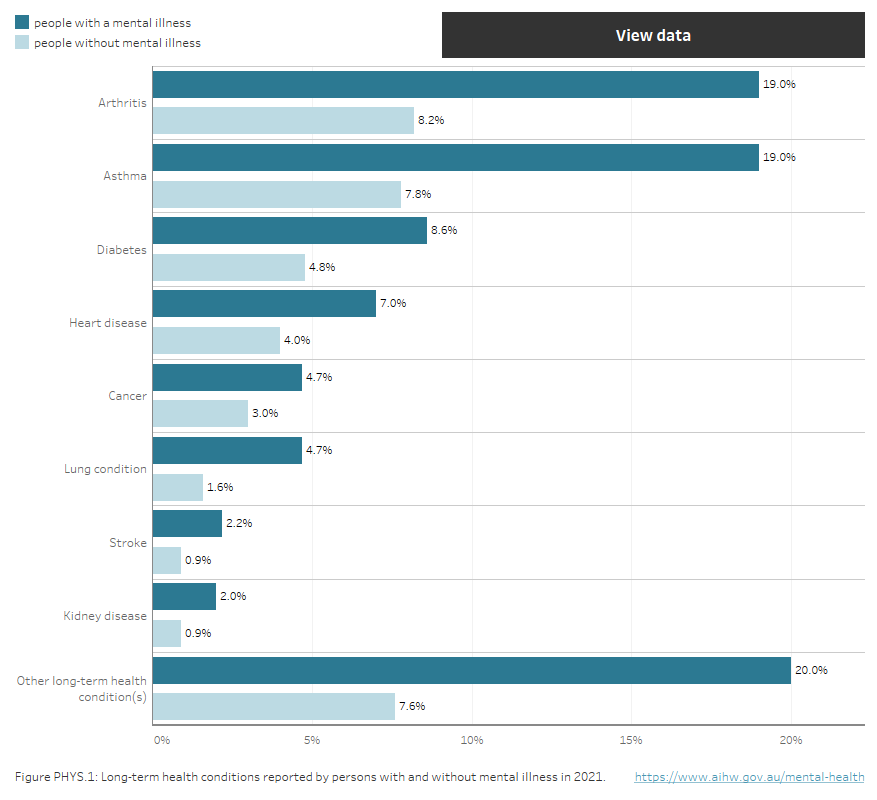
The 2021 Australian Census results – which include people of all ages – showed a notable overlap between physical health and mental health problems: people who reported having a mental illness were more likely to report having a long-term health condition (Figure PHYS.1) (ABS 2022). Among the most common long-term conditions reported by those with a mental illness were arthritis, asthma and diabetes (Figure PHYS.1). Furthermore, given that the Census relies on people self-reporting conditions, this is likely to be an underestimate as many people did not respond to this item or may not be aware that they have a long-term health condition. Refer to Chronic conditions and multimorbidity for more information.
Figure PHYS.1: Long-term health conditions reported by persons with and without mental illness in 2021
Horizontal bar chart showing percentages of people with a mental illness and people without a mental illness who reported long-term health conditions (excluding mental illness) in the 2021 Census. Across all long-term health condition categories, proportions of people with long-term health conditions are higher among people with mental illness.
Notes
- Mental illness includes anxiety and depression.
- Diabetes excludes gestational diabetes; Cancer includes remission; Heart Disease includes heart attack and angina; Lung condition includes Chronic obstructive pulmonary disease (COPD) or emphysema; Other long-term health condition(s)’ excludes dementia, Alzheimer’s disease and mental illness.
Source: ABS 2022.
A recent study of Australian general practice records examined the prevalence of physical health conditions and biomedical risk factors among people with SMI. Similarly, it showed a notable overlap between mental and physical illness (Belcher et al. 2021). The prevalence of all surveyed biomedical risk factors was higher among patients with SMI than patients without. These included:
- dyslipidaemia (high cholesterol) (25% among those with SMI compared with 18% in patients without)
- hypertension (27% compared with 22%)
- obesity (29% compared with 19%).
The prevalence of all surveyed physical conditions was also higher among patients with SMI than patients without. These included:
- back pain (35% among those with SMI compared with 19% in patients without)
- cardiovascular disease (10% compared with 6.7%)
- gastro-oesophageal reflux disease (29% compared with 15%)
- arthritis (27% compared with 19%)
- cancer (19% compared with 15%).
Almost three-quarters (71%) of patients with SMI had at least one of the surveyed physical health conditions, compared with over half (54%) of people without.
The second national survey of People Living with Psychotic Illness also provided estimates on the physical health of Australians living with a psychotic illness (Morgan et al. 2012). Chronic back, neck or other pain was the most common chronic physical condition (32% compared with 28% for the general population) identified among people with a psychotic illness in 2010. Other common conditions included asthma (30% compared with 20% for the general population) and heart or circulatory conditions (27% compared with 16%).
In 2010, one-quarter (24%) of people with a psychotic illness were at high risk of cardiovascular disease, almost half (45%) were obese and almost two-fifths (38%) reported gaining weight as a medication side effect. Physical activity levels were markedly lower in people with a psychotic illness, with 96% classified as either sedentary or undertaking low levels of exercise in the previous week compared with 72% for the general population (Morgan et al. 2012).
Causes of physical illness among people with mental illness
Mental health is known to affect physical health. For example, there is a long-established association between depression and heart disease. Multiple studies across various types of populations have shown that people with depression but no history of heart disease when the depression is assessed are at markedly higher risk for coronary heart disease or cardiac mortality (Carney and Freedland 2003). Similarly, among patients who have just experienced a major cardiac event, such as a heart attack, those with depression are at an increased risk of another cardiac event or cardiac mortality compared to non-depressed patients (Dhar and Barton 2016). While the association between the depression and coronary heart disease is well known, researchers have only recently begun to understand the biological mechanisms behind this relationship (Dhar and Barton 2016). Yet the reasons people with mental illness and especially SMI are more likely to experience poorer physical health and reduced life expectancy compared to the general population go beyond the physiological changes associated with mental illness.
According to the Royal Australian and New Zealand College of Psychiatrists, the reasons people living with severe mental illness experience poorer physical health include:
- greater exposure to the known risk factors for physical disease such as lower socio-economic status, smoking, poor nutrition, reduced physical activity and higher sedentary behaviour
- reduced access to and quality of health care due to financial barriers, and stigma and discrimination among health care providers
- systemic issues in health care delivery, especially the separation of mental and physical health services, and a lack of clarity about who is responsible for monitoring the physical health of people with serious mental illness
- adverse effects of psychotropic medication, in particular their contribution to metabolic syndrome, obesity, cardiovascular disease and type 2 diabetes
- impacts from polypharmacy (the prescription of multiple medications) and prescribing practices
- lack of capability among both generalist and specialist health care staff to deal with complex comorbidities – mental health staff may lack skills, training and confidence to treat physical conditions and vice versa for physical health teams (RANZCP 2015).
For some people living with mental illness, symptoms may interfere with receiving medical care or compromise effective communication of physical symptoms with health care workers (Melamed et al. 2019).
In addition to poorer physical health and shorter life expectancy, higher rates of physical comorbidity among people with SMI can lead to higher levels of ongoing disability, reduced participation in the workforce and a greater likelihood of poverty and welfare dependency (RANZCP 2015).
Life expectancy
That people living with mental illness have a reduced life expectancy compared with the general population has been extensively documented around the world (Chang et al. 2011; Walker et al. 2015; Plana-Ripoll et al. 2019). Research from Western Australia found that the gap in life expectancy for people with mental illness registered with West Australian mental health services compared with the general population in 2005 was 15.9 years for men and 12.0 years for women (Lawrence et al. 2013). This research also indicated that the mortality gap for people living with mental illness had increased from 1985, by 2.5 years for men and 1.6 years for women since 1985, with the increase largely driven by gains in life expectancy for the general population (Lawrence et al. 2013) . This finding aligns with studies from other high-income countries suggesting that the mortality gap for people with mental illness may be increasing over time, in part due to gains in life expectancy for the general population not experienced (or at least not experienced in equal measure) by those with mental illness and especially SMI (Neilsen et al 2013; Hayes et al 2017; Laursen et al 2019).
Rather than a direct result of mental illness or death by suicide, almost 80% of premature deaths of people with mental illness are due to potentially preventable physical health comorbidities (Lawrence et al. 2013). These include type 2 diabetes, respiratory diseases, cancer and cardiovascular disease (De Hert et al. 2009). Compared to the general population, people with SMI have a 2- to 3-fold risk of developing hypertension and metabolic syndrome and, if under the age of 50, a 3-fold risk of dying from coronary heart disease (De Hert et al. 2009; Osborn et al. 2007). If diagnosed with cancer, people living with SMI experience higher rates of mortality compared to the general population (Launders et al. 2022; Charlesworth et al. 2023).
Substance use and mental illness
Use of alcohol, tobacco and illicit drugs can trigger or worsen mental health issues and are strongly associated with physical health conditions including cancer, cirrhosis, and cardiovascular disease (AIHW 2022).
The relationship between mental illness and substance use is complex. A mental illness may make a person more likely to use drugs as an attempt to self-medicate symptoms associated with their mental illness. Conversely, substance use may be a contributing factor for the initial symptoms of mental illness. Certain substances may cause a substance-induced psychosis which can last for days or weeks after the end of intoxication. However, if someone has a pre-disposition to developing a psychotic illness, such as schizophrenia, the use of illicit drugs may bring on the first episode of what can be a longer-lasting psychotic illness (NDARC 2011). Critically, this does not mean that mental illness necessarily causes substance use and vice versa: common risk factors (such as trauma, personality traits, genetic influences and the childhood environment) may cause substance use and mental illness to independently develop in the same individual (UNODC 2022).
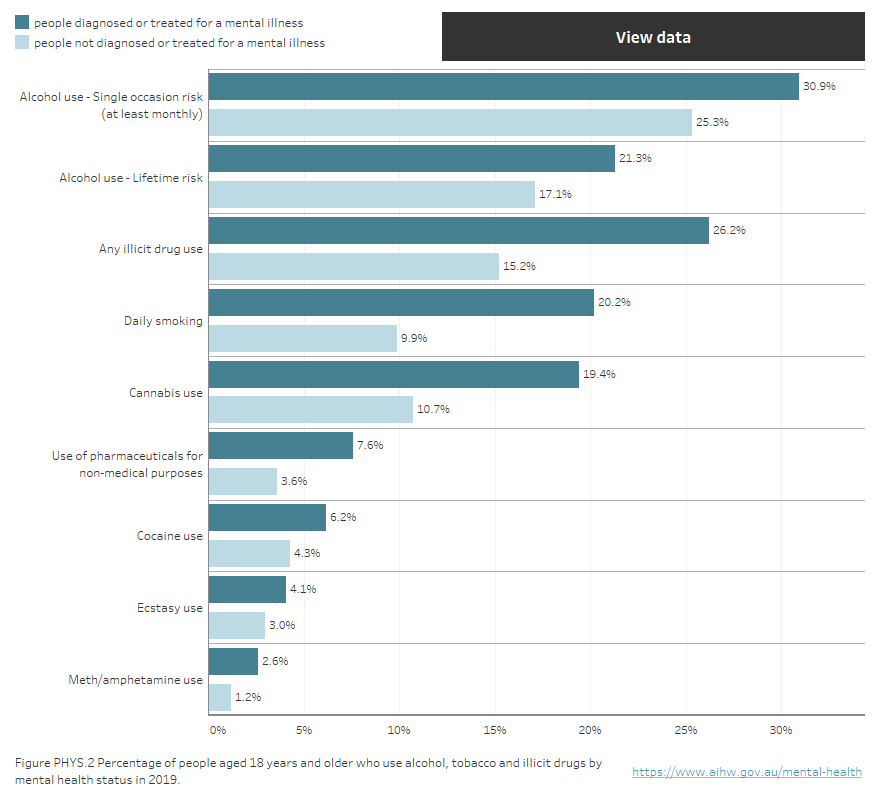
Among people living with mental illness, there are higher rates of alcohol, tobacco and other drug use compared with people without mental illness (refer to Figure PHYS.2).
According to the 2019 National Drug Strategy Household Survey (NDSHS) (AIHW 2020), people who were diagnosed or treated for a mental illness in the previous 12 months were about 20% more likely to report recent or lifetime drinking at risky levels than people who had not (Figure PHYS.2). Similarly, Australian general practice records in 2021 showed that the prevalence of moderate to heavy drinking among patients with SMI was more than double that for the population without (4.7% compared with 2.3%) (Belcher et al. 2021). For more information on alcohol use, refer to Alcohol.
In the NDSHS, people who reported a mental illness were twice as likely to smoke daily as those who had not been diagnosed with, or treated for, a mental illness (20% compared with 9.9%; Figure PHYS.2) (AIHW 2020). Likewise, according to Australian general practice records, 47% of people with SMI are current or past smokers, compared with about 30% of the population without (Belcher et al. 2021). Two-thirds (66%) of people with psychosis smoke, with an average of 21 cigarettes per day (Morgan et al. 2012). For more information on Tobacco use, refer to Tobacco and e-cigarettes.
Illicit drug use is also more common among people with mental illness. In the NDSHS, compared with people with no mental illness, people with a mental illness were 1.7 times as likely to have used any illicit drug in the previous 12 months and about twice as likely to have used meth/amphetamine and prescription pharmaceuticals for non-medical purposes (Figure PHYS.2) (AIHW 2020). The lifetime rate of any illicit substance use or dependence in people with psychosis was at 55%, 6 times the general population rate of 9% (Morgan et al. 2012). For more information on illicit drug use, refer to Illicit drug use.
Figure PHYS.2 Proportion of people aged 18 years and over who use alcohol, tobacco and illicit drugs by mental health status in 2019
Horizontal bar chart showing percentage of people aged 18 years and older in 2019 who used alcohol, tobacco and illicit drugs according to whether in the previous 12 months they had been (a) diagnosed or treated for a mental illness or (b) not diagnosed or treated for a mental illness. Across all substance use categories (Alcohol use – Lifetime risk; Alcohol use – Single occasion risk [at least monthly]; Any illicit drug use; Cannabis use; Cocaine use; Ecstasy use; Daily smoking; Meth/Amphetamine use; Use of pharmaceuticals for non-medical purposes) the percentage of people reporting substance use is higher among those diagnosed or treated for a mental illness.
Notes
- Mental illness includes depression, anxiety disorder, schizophrenia, bipolar disorder, an eating disorder and other forms of psychosis.
- Alcohol data are reported against the 2009 Australian alcohol guidelines.
- ‘Lifetime risk’ is defined as the accumulated risk from drinking either on many drinking occasions, or on a regular (for example, daily) basis over a lifetime. Drinking no more than 2 standard drinks on any day reduces the lifetime risk of harm from alcohol-related disease or injury.
- ‘Single occasion risk’ refers to more than 4 standard drinks on a single occasion.
Source: AIHW 2020.
Comorbidity between substance use disorder – which itself is categorised as a mental disorder – and other kinds of mental disorders is common (Mills et al. 2019). According to the NSMHW 2020–2022, while 8.8% of people who met the diagnostic criteria for an anxiety or affective disorder also met the criteria for a substance use disorder, almost half (46%) of people who met the diagnostic criteria for substance use disorder also met the criteria for an anxiety or affective disorder (ABS 2023).
While mental illness is associated with a reduced life expectancy, research has shown that comorbid substance use disorder alongside other mental disorders is associated with markedly higher mortality rates and larger reductions in life expectancy (Plana-Ripoll et al. 2020).
For more information, refer to Alcohol, tobacco and other drug use among people with mental health conditions.
Impact of COVID-19 on people living with mental illness
A number of data sources have indicated impacts on both the mental and physical health of Australians during the pandemic. As in other parts of the world, the pandemic and related restrictions had significant impacts on the mental health of Australians. Multiple sources of data indicated increased and more widespread psychological distress compared with pre-pandemic levels and increased use of mental health services and mental health prescriptions (ABS 2021; Biddle and Gray 2021; Butterworth 2020; AIHW 2023). Those aged 18–35 years, women, people with a disability, renters, and people who report having a mental health condition were more likely to report high or very high levels of psychological distress (ABS 2021).
Despite modifications and additions to health service delivery models during the pandemic (for example, telehealth consultations), many people delayed access to health care which can lead to acute and long-term health consequences for individuals (White et al. 2021). Issues included restrictions on movement during lockdowns, fear of contracting COVID-19, fear of overburdening the health system, financial stress and disruptions to elective surgery and other health services. Notably, people experiencing high levels of psychological distress were 6 times more likely to choose not to consult a health professional when needed than those who were not (Zhang et al. 2020).
For people living with SMI – a group which generally has less access to health care – pandemic-related restrictions may have worsened physical health due to challenges particularly affecting this group (Melamed et al. 2020). People with SMI were already overrepresented in acute physical health care episodes in hospitals prior to the pandemic, therefore the burden placed on acute health care settings from the pandemic may have disproportionally affected this group (Melamed et al. 2020; Sara et al. 2021).
Future directions
Data linkage, for example through the National Integrated Health Services Information (NIHSI) data asset (also known as the National Health Data Hub), may provide further insights into the relationships between mental illness and physical comorbidities among the Australian population. While separate data collections provide a limited view on peoples’ overall health, data linkage between collections allows for analysis of the impact of mental illness on physical health conditions from across different service settings and types of service usage. This data could assist in identifying areas of disadvantage in broader health settings and barriers to service usage for people with mental illness, which is critical as this population group accesses health services at a lower rate than the general population.
Where can I find more information?
For more information on the physical health of people with mental illness, refer to:
- Equally Well Improving the physical health of people living with mental illness
- Victoria University Being equally well: A national policy roadmap to better physical health care and longer lives for people living with serious mental illness
- The Royal Australian & New Zealand College of Psychiatrists Keeping body and mind together: improving the physical health and life expectancy of people with serious mental illness
- World Health Organization (WHO) Management of physical health conditions in adults with severe mental disorders, WHO Guidelines
| Key concept | Description |
|---|---|
Comorbidity | Comorbidity refers to occurrence of more than 1 condition/disorder at the same time. Comorbidity is common among those with mental illness. It can involve more than 1 mental disorder, or 1 mental disorder and 1 or more physical conditions. |
Data linkage | Data linkage brings together information derived from different sources but relating to the same individual, place or event in a single file. Data linkage has been used for studies of epidemiology, health service outcomes and use, and needs analysis. |
Metabolic syndrome | Metabolic syndrome is an accumulation of health conditions, which together raise the risk of an individual developing atherosclerotic cardiovascular disease, insulin resistance, and diabetes mellitus, and vascular and neurological complications such as a cerebrovascular accident. |
Mortality gap | Mortality gap is the disparity in life expectancy between the general population and a specific group of interest. |
Severe mental illness (SMI) | Severe mental illness – often used interchangeably with the terms serious mental illness and severe and persistent mental illness – commonly includes diagnoses of schizophrenia, major affective disorders and some personality disorders resulting in lifelong disabling conditions that severely impair personal and social functioning, and require ongoing and long-term support and treatment. These terms lack consensus definition but are commonly characterised by the combination of diagnosis, disability and duration (see Zumstein and Riese 2020). |
Substance use disorder | Substance use disorder is the persistent use of drugs (including alcohol and tobacco) despite serious harms and negative consequences associated with their use. In the International Statistical Classification of Diseases and Related Health Problems,10th revision, substance use disorders come under the block Mental and behavioural disorders due to psychoactive substance use. This block contains a wide variety of disorders that differ in severity and clinical form but that are all attributable to the use of one or more psychoactive substances, which may or may not have been medically prescribed. |
ABS (Australian Bureau of Statistics) (2021) Household Impacts of COVID-19 Survey, June 2021, ABS, Australian Government, accessed 18 January 2024.
ABS (2022) Type of Long-term Health Condition (LTHP) by Whether has Mental Health Condition (HMHCP) [Census Table Builder], accessed 18 January 2024.
ABS (2023) National Study of Mental Health and Wellbeing, 2020-21: Summary of results, ABS, Australian Government, accessed 12 October 2023.
AIHW (Australian Institute of Health and Welfare) (2020) National Drug Strategy Household Survey 2019, AIHW, Australian Government, accessed 15 October 2022.
AIHW (2022) Alcohol, tobacco & other drugs in Australia, Health Impacts, AIHW, Australian Government, accessed 12 December 2023.
AIHW (2023) Mental health services activity monitoring quarterly data, AIHW, Australian Government, accessed 12 October 2023.
Belcher J, Myton R, Yoo J, Boville C and Chidwick K (2021) Exploring the physical health of patients with severe or long-term mental illness using routinely collected general practice data from MedicineInsight, Australian Journal of General Practice, 50(12):944–949, doi:10.31128/AJGP-08-20-5563.
Biddle N and Gray M (2021) Tracking wellbeing outcomes during the COVID-19 pandemic (October 2021): Putting the worst behind us?, Australian National University, accessed 15 March 2022.
Butterworth P (2020) Research Insight 6/20 How to protect mental health through the COVID-19 crisis?, University of Melbourne, accessed 15 March 2022.
Carney RM and Freedland KE (2003) Depression, mortality, and medical morbidity in patients with coronary heart disease, Biological Psychiatry, 54(3):241-7. doi: 10.1016/s0006-3223(03)00111-2.
Chang CK, Hayes RD, Perera G, Broadbent MTM, Fernandes AC, Lee WE, Hotopf, M and Stewart R (2011) Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London PLoS ONE, 6(5): e19590, doi: 10.1371/journal.pone.0019590
Charlesworth L, Fegan C and Ashmore R (2023) How does severe mental illness impact on cancer outcomes in individuals with severe mental illness and cancer? A scoping review of the literature, J Med Imaging Radiat Sci, 54(2S):S104-S114. doi:10.1016/j.jmir.2023.01.007.
De Hert M, Dekker JM, Wood D, Kahl KG, Holt RI and Möller HJ (2009) Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC), Eur Psychiatry, 24(6):412-24, doi: 10.1016/j.eurpsy.2009.01.005.
Dhar AK and Barton DA. ‘Depression and the Link with Cardiovascular Disease’, Front Psychiatry, 7:33, doi: 10.3389/fpsyt.2016.00033.
Firth J, Siddiqi N, Koyanagi A, Siskind D, Rosenbaum S, Galletly C, Allan S, Caneo C, Carney R, Carvalho AF, Chatterton ML, Correll CU, Curtis J, Gaughran F, Heald A, Hoare E, Jackson SE, Kisely S, Lovell K, Maj M, McGorry PD, Mihalopoulos C, Myles H, O'Donoghue B, Pillinger T, Sarris J, Schuch FB, Shiers D, Smith L, Solmi M, Suetani S, Taylor J, Teasdale SB, Thornicroft G, Torous J, Usherwood T, Vancampfort D, Veronese N, Ward PB, Yung AR, Killackey E and Stubbs B (2019) The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness, The Lancet Psychiatry, 6(8):675–712, doi:10.1016/S2215-0366(19)30132-4.
Hayes JF, Marston L, Walters K, King MB and Osborn DPJ (2017) Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000-2014, Br J Psychiatry, 211(3):175-181. doi: 10.1192/bjp.bp.117.202606.
Launders N, Scolamiero L, Osborn DPJ and Hayes JF (2022) Cancer rates and mortality in people with severe mental illness: Further evidence of lack of parity, Schizophr Res. 246:260-267, doi: 10.1016/j.schres.2022.07.008.
Laursen TM, Plana-Ripoll O, Andersen PK, McGrath JJ, Toender A, Nordentoft M, Canudas-Romo and Erlangsen A (2019) Cause-specific life years lost among persons diagnosed with schizophrenia: Is it getting better or worse? Schizophr Res, 206:284-290. doi: 10.1016/j.schres.2018.11.003.
Lawrence D, Hancock K and Kisely S (2013) The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers’, British Medical Journal, 346:f2539, doi:10.1136/bmj.f2539.
Melamed OC, Fernando I, Soklaridis S, Hahn MK, LeMessurier KW and Taylor VH (2019) Understanding engagement with a physical health service: A qualitative study of patients with severe mental illness, Can J Psychiatry, (12):872-880, doi: 10.1177/0706743719862980.
Melamed OC, Hahn MK, Agarwal SM, Taylor VH, Mulsant BH and Selby P (2020) Physical health among people with serious mental illness in the face of COVID-19: Concerns and mitigation strategies, Gen Hosp Psychiatry, 66:30-33. doi: 10.1016/j.genhosppsych.2020.06.013.
Mills K, Marel C, Madden E and Teesson M (2019) Lessening the Burden of Comorbid Substance Use and Mental Disorders Through Evidence-Based Care: The Case for a National Minimum Qualifications Strategy Submission to the Australian Government Productivity Commission Mental Health Inquiry, Matilda Centre for Research in Mental Health and Substance Use, University of Sydney, Sydney, accessed 23 October 2023.
Morgan VA, Waterreus A, Jablensky A, Mackinnon A, McGrath JJ, Carr V, Bush R, Castle D, Cohen M, Harvey C, Galletly C, Stain HJ, Neil AL, McGorry P, Hocking B, Shah S and Saw S (2012) People living with psychotic illness 2010: The second Australian national survey Aust N Z J Psychiatry, 46(8):735-52, doi: 10.1177/0004867412449877.
National Drug and Alcohol Research Centre (NDARC) (2011) Psychosis + Substance Use [booklet] University of NSW, Sydney.
Nielsen RE, Uggerby AS, Jensen SO and McGrath JJ (2013) Increasing mortality gap for patients diagnosed with schizophrenia over the last three decades--a Danish nationwide study from 1980 to 2010, Schizophr Res,146(1-3):22-7, doi: 10.1016/j.schres.2013.02.025
Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A and King MB (2007) Relative Risk of Cardiovascular and Cancer Mortality in People With Severe Mental Illness From the United Kingdom's General Practice Research Database, Arch Gen Psychiatry, 64(2):242–249, doi:10.1001/archpsyc.64.2.242
Plana-Ripoll O, Pedersen CB, Agerbo E, Holtz Y, Erlangsen A, Canudas-Romo V, Andersen PK, Charlson FJ, Christensen MK, Erskine HE, Ferrari AJ, Iburg KM, Momen N, Mortensen PB, Nordentoft M, Santomauro DF, Scott JG, Whiteford HA, Weye N, McGrath JJ and Laursen TM (2019) A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study’, Lancet, 394(10211):1827-1835, doi: 10.1016/S0140-6736(19)32316-5.
Plana-Ripoll O, Musliner KL, Dalsgaard S, Momen NC, Weye N, Christensen MK, Agerbo E, Iburg KM, Laursen TM, Mortensen PB, Pedersen CB, Petersen LV, Santomauro DF, Vilhjálmsson BJ, Whiteford HA and McGrath JJ (2020) Nature and prevalence of combinations of mental disorders and their association with excess mortality in a population-based cohort study, World Psychiatry 19(3):339-349. doi: 10.1002/wps.20802.
RANZCP (Royal Australian and New Zealand College of Psychiatrists) (2015) Keeping body and mind together: Improving the physical health and life expectancy of people with serious mental illness, A report prepared for the Royal Australian and New Zealand College of Psychiatrists, RANZCP, accessed 13 March 2022.
Sara G, Chen W, Large M, Ramanuj P, Curtis J, McMillan F, Mulder CL, Currow D and Burgess P (2021) Potentially preventable hospitalisations for physical health conditions in community mental health service users: a population-wide linkage study, Epidemiology and Psychiatric Sciences, 30(e22):1-10, doi: 10.1017/S204579602100007X.
UNODC (United Nations Office on Drugs and Crime) (2022) Comorbidities in drug use disorders: No wrong door, Discussion paper, UN, accessed 17 October 2013.
Walker ER, McGee RE and Druss BG (2015) Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis, JAMA Psychiatry, 72(4):334–341, doi:10.1001/jamapsychiatry.2014.2502.
White J, Cavenagh D, Byles J, Mishra G, Tooth L and Loxton D (2021) The experience of delayed health care access during the COVID 19 pandemic in Australian women: A mixed methods exploration, Health & Social Care in the Community, 00:1–12, doi:10.1111/hsc.13546.
Zhang Y, Liu J and Scott A (2020) Research Insight 23/20: Using health care during the pandemic: Should I stay or should I go? University of Melbourne, accessed 15 March 2022.
Zumstein N and Riese F (2020) Defining Severe and Persistent Mental Illness-A Pragmatic Utility Concept Analysis Front Psychiatry 11:648. doi:10.3389/fpsyt.2020.00648
This section was last updated 14 February 2024