Reason for hospitalisation
A person’s principal diagnosis reflects the specific reason they were admitted to hospital and additional diagnoses reflect conditions that impacted care needs during their admission. On this page, the principal diagnosis is summarised using the principal diagnosis group, which reflects the broad category of disease or health problem that the person needed treatment for.
The proportion of people with a principal or additional diagnosis of dementia is reported, reflecting people who were hospitalised due to their dementia or whose dementia impacted the care they required.
Principal diagnosis group
The most common reason that people living with dementia were hospitalised was for:
- 20% injury or poisoning (most often due to fracture of subcapital section of femur)
- 13% respiratory diseases (most often due to pneumonia –unspecified)
- 11% circulatory diseases (most often due to congestive heart failure).
Injury or poisoning, respiratory diseases and circulatory diseases were the most common reason for hospitalisation among community-dwellers who died, aged care residents who died and aged care residents, though the most common principal diagnosis varied (Figure 8 and Table S1.11).
For community-dwellers, the most common reasons for hospitalisation were injury or poisoning, other signs and symptoms (most often due to syncope and collapse) and circulatory diseases.
For people who transitioned to live in residential aged care the most common reasons for hospitalisation were injury or poisoning, mental and behavioural disorders (most often due to delirium superimposed on dementia) and circulatory diseases.
Figure 8 Top principal diagnosis groups for people living with dementia, by change in usual residence or mortality within 7-days of discharge
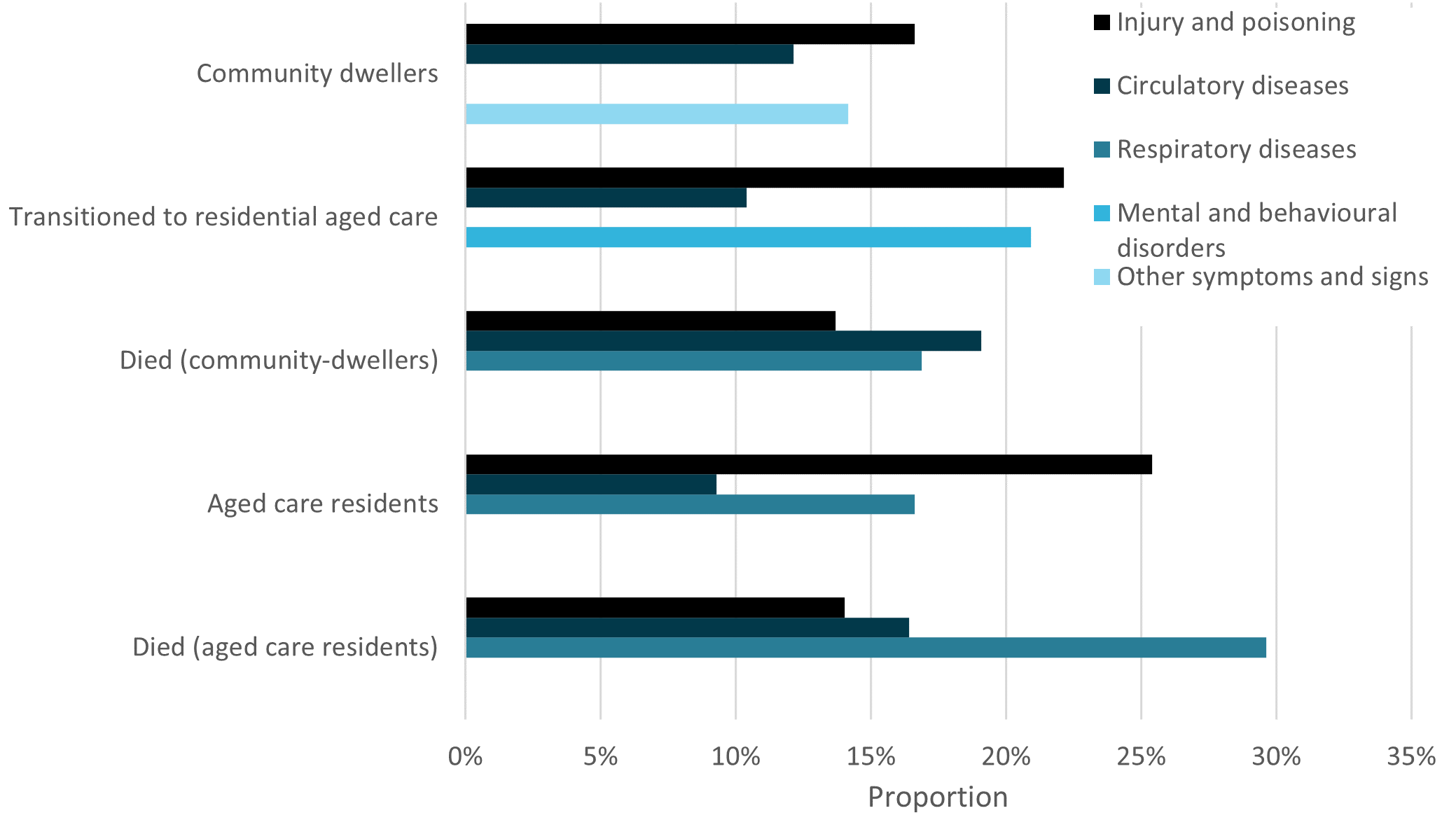
Source: AIHW NIHSI 2018–19, analysis of NIHSI.
Hospitalised due to or with dementia
Most people living with dementia did not have dementia recorded as a principal or additional diagnosis (58%). Only 10% of people living with dementia were hospitalised due to dementia and 32% had dementia recorded as a condition that affected the care they required during their hospitalisation (Table S1.12). This shows the importance of linked data for identifying people with dementia.
The proportion of people who were hospitalised due to dementia was highest for people who transitioned to residential aged care (26%) and lowest for aged care residents (5%) and aged care residents who died (5%). This suggests that people who lived in the community prior to their hospitalisation may require additional support in the community to manage their dementia.
The proportion of people whose dementia impacted their care but was not the main reason for admission was highest for community-dwellers who died (48%) and lowest for aged care residents (31%) and community-dwellers (29%).
Figure 9 Proportion of people who were hospitalised due to or with dementia, by change in usual residence or mortality within 7-days of discharge
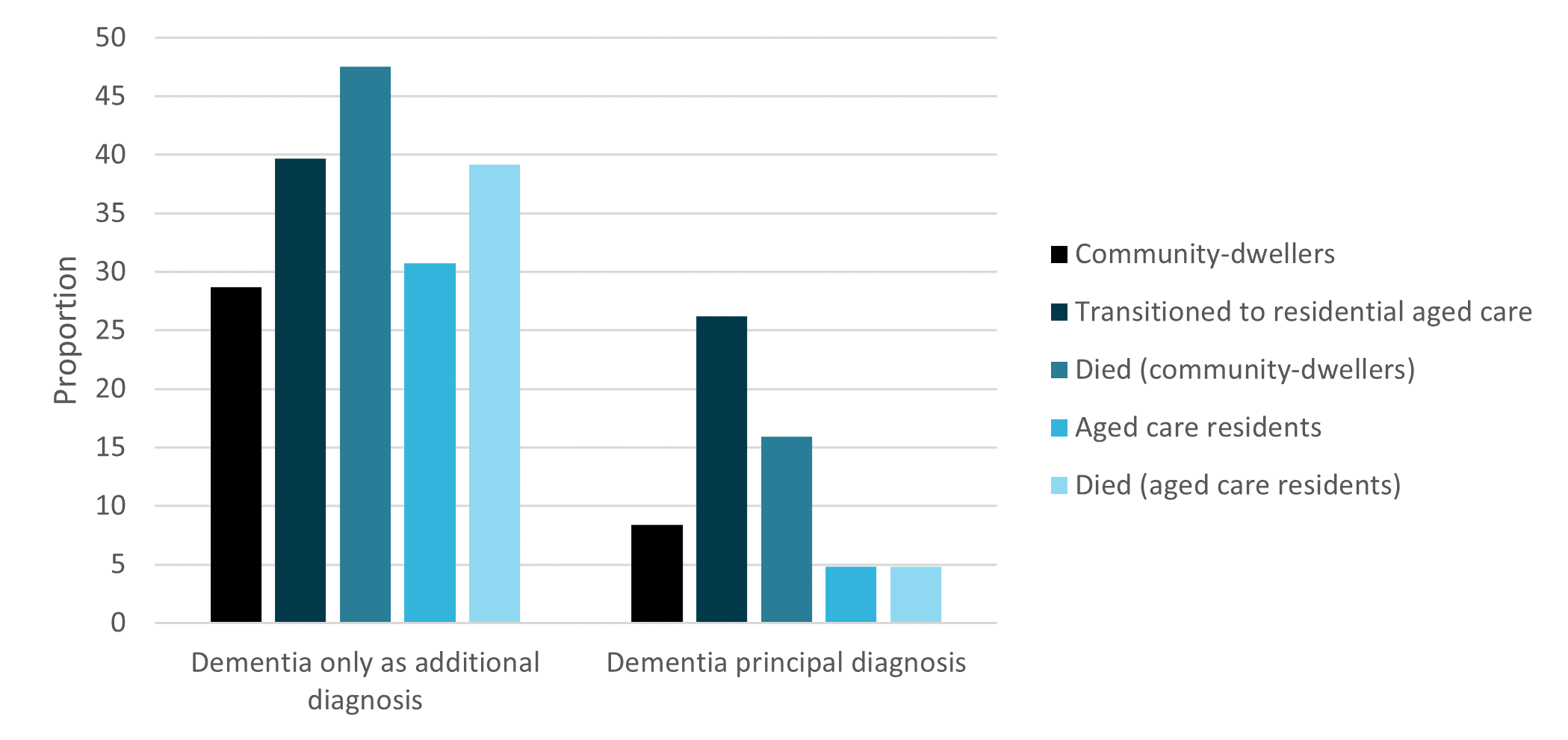
Source: AIHW NIHSI 2018–19, analysis of NIHSI.


