Patient experiences
This section presents data for the patient experience indicators supplied by Australia to the HCQO collection. It compares these data with the HCQO results for other OECD countries, and comments on the comparability of the data provided to the OECD specification (OECD 2021).
The OECD published all patient experience indicators in OECD.Stat and a selection of patient experience indicators in Health at a glance 2023. Australia calculated and submitted 4 out of 13 of the patient experience indicators requested:
- consultation skipped to costs
- medical tests, treatment or follow-up skipped due to costs
- prescribed medicines skipped due to costs
- doctor spending enough time with patients during the consultation.
See Patient experiences indicator definitions.
Overall data comparability and methods
The most recent data supplied by Australia for the patient experience indicators were for 2020–21 and 2021–22. The data are recorded as 2020 and 2021 data in the OECD.Stat database, and so are described in that way here. These data were extracted from the OECD.Stat database in January 2024, and may not reflect subsequent updates made to the database.
The OECD requested patient experiences data for adults aged 16 and over, disaggregated by age and sex. The OECD then calculated age-sex standardised rates (standardised to the equivalent 2015 OECD population) for these indicators based on the supplied data. The indicators are presented on the same basis here.
The ABS Patient Experience Survey is an annual survey that is used to collect information from people aged 15 and over about their experiences with selected aspects of the health system over the last 12 months. For the ‘consultation skipped’ indicator, the ABS survey asked people a number of questions about their experiences with GPs, medical specialists, dental professionals or hospitals, whereas the OECD HCQO requested information in relation to experiences with ‘a health professional’ (for example, a doctor, nurse or allied health professional). Therefore, the wording used by the ABS in the Patient Experience Survey differs from the OECD specifications.
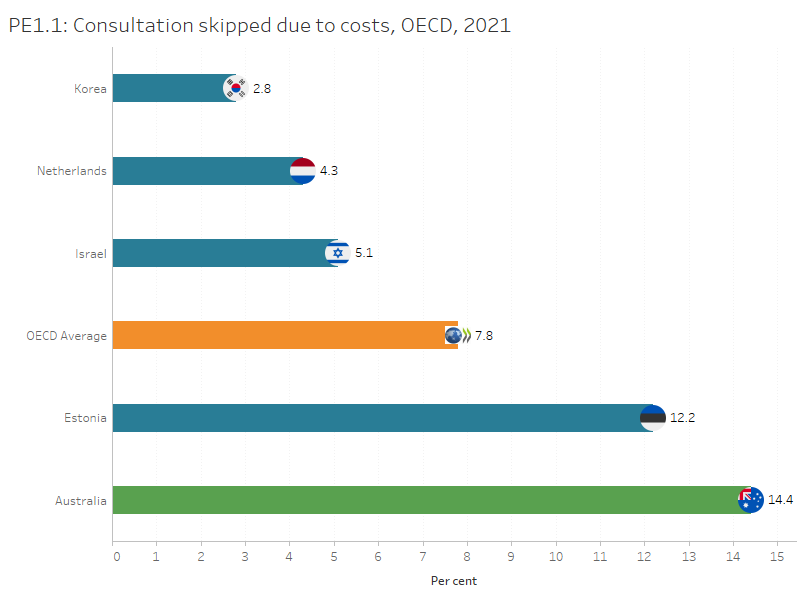
Consultations skipped due to costs
This indicator was supplied using multiple questions from the ABS Patient Experience Survey that asked people whether there had been any time they needed to go to a GP, medical specialist, dental professional or hospital but did not go, or delayed going, due to the cost.
In Australia, 14% of people aged 16 and over skipped a consultation due to costs in 2021, almost twice the OECD average of 7.8% of people aged 16 and over. Among the countries that reported 2021 data for this indicator, Australia had the highest proportion while Korea had the lowest proportion of people that skipped a consultation due to costs (2.8% of people 16 years and over).
In Australia, the percentage of people aged 16 and over skipped a consultation due to costs was higher for females (16%) than males (13%). This rate has fluctuated over time in the past decade, ranging from 8.9% in 2016 to 19% in 2012.
Interactive PE1 below presents Australia’s 10-year trend for this indicator where data are available.
Figures PE1.1 and PE1.2
The figure presents Australia’s 10-year trend for ‘Consultations skipped due to costs’ indicator. The rate has fluctuated over time.
Refer to the Data tables for more information.
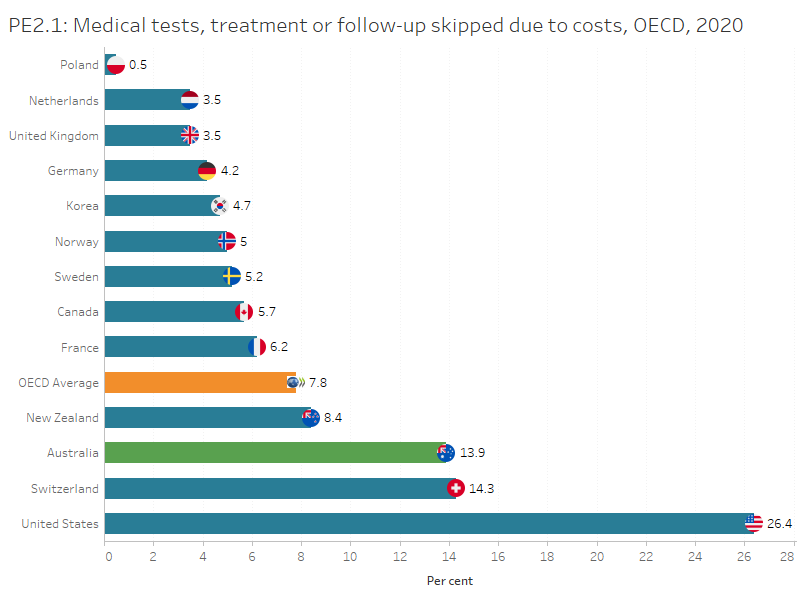
Medical tests skipped due to costs
This indicator was supplied using multiple questions from the ABS Patient Experience Survey that asked people whether they delayed, or did not get, referred pathology or imaging tests due to the cost. Data for this indicator was not collected in the 2021 ABS patient experience survey, so the data from 2020 is presented below.
In Australia, 14% of people aged 16 years and over delayed or skipped a pathology or imaging test due to costs, almost twice the OECD average of 7.8%. Among countries that reported 2020 data for this indicator, Poland had the lowest proportion of people that skipped a pathology or imaging test due to costs (0.5% of people 16 years and over).
In Australia, the rate of people who delayed or skipped a pathology or imaging test due to costs has varied over the past decade, ranging from 3.0% in 2018 to 14% in 2020. This percentage was higher for females (17%) than males (10%).
Interactive PE2 below presents Australia’s 10-year trend for this indicator where data are available.
Figures PE2.1 and PE2.2
The figure presents Australia’s 10-year trend for ‘Medical tests skipped due to costs’ indicator.
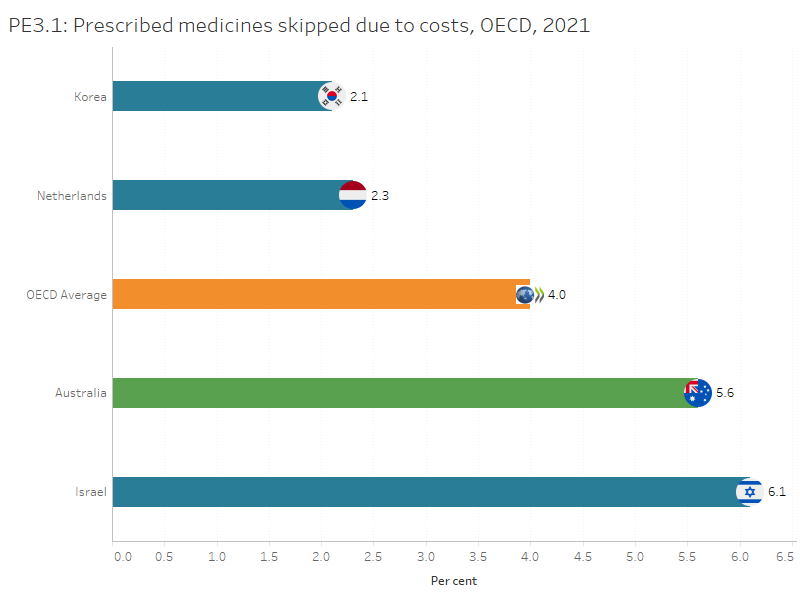
Prescribed medicines skipped due to costs
This indicator was supplied using the ABS Patient Experience Survey question that asked whether people delayed or did not get a prescription due to the cost.
In Australia, 5.6% of people aged 16 and over delayed or skipped prescribed medicines due to costs in 2021, higher than the OECD average of 4% of people aged 16 and over. Among countries that reported 2021 data for this indicator, Korea had the lowest proportion of people that skipped prescribed medicines due to costs (2.1% of people 16 years and over).
In Australia, the percentage of people aged 16 and over that skipped prescribed medicines due to costs has reduced in 2021 (5.6% in 2021 as compared to 8.5% in 2020) The proportion was higher for females (6.1%) than males (5.1%).
Interactive PE3 below presents Australia’s 10-year trend for this indicator where data are available.
Figures PE3.1 and PE3.2
The figure presents Australia’s 10-year trend for ‘Prescribed medicines skipped due to costs’ indicator. The rate has remained stable since 2016.
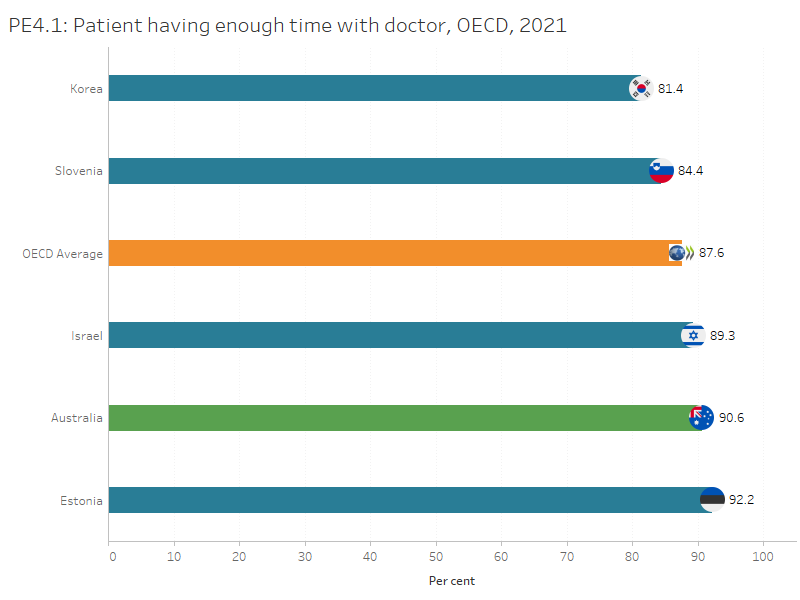
Patient having enough time with doctor
This indicator was supplied using a question from the ABS Patient Experience Survey that asked those people who saw a GP for their own health about whether the doctor(s) spent enough time with the respondents during the consultation for the OECD HCQOs.
In Australia, 91% of patients aged 16 and over reported that for all the GPs seen in the past 12 months, the doctor had always or often spent enough time with them in 2021, higher than the OECD average of 88% of patients aged 16 and over. Among countries that reported 2021 data for this indicator, Estonia had the highest proportion of people that reported that a doctor spent enough time with them (92% of people 16 years and over)
In Australia this rate has remained relatively stable since 2013. The proportion was slightly higher for males (92%) than females (89.5%).
The OECD recommends monitoring patient experience with any doctor, as Australia has done, but some of the other countries to which Australia is compared measure experience with a patient’s regular doctor (OECD 2021).
Interactive PE4 below presents Australia’s 10-year trend for this indicator where data are available.
Figures PE4.1 and PE4.2
PE4.1 presents Australia’s 10-year trend for ‘Patient having enough time with doctor’ indicator. The rate has remained stable since 2013.
Refer to the Data tables for more information.
References
OECD 2023. Health at a glance 2023: OECD indicators. Paris: OECD.


