Health of young people
Citation
AIHW
Australian Institute of Health and Welfare (2024) Health of young people, AIHW, Australian Government, accessed 26 April 2024.
APA
Australian Institute of Health and Welfare. (2024). Health of young people. Retrieved from https://pp.aihw.gov.au/reports/children-youth/health-of-young-people
MLA
Health of young people. Australian Institute of Health and Welfare, 16 April 2024, https://pp.aihw.gov.au/reports/children-youth/health-of-young-people
Vancouver
Australian Institute of Health and Welfare. Health of young people [Internet]. Canberra: Australian Institute of Health and Welfare, 2024 [cited 2024 Apr. 26]. Available from: https://pp.aihw.gov.au/reports/children-youth/health-of-young-people
Harvard
Australian Institute of Health and Welfare (AIHW) 2024, Health of young people, viewed 26 April 2024, https://pp.aihw.gov.au/reports/children-youth/health-of-young-people
Get citations as an Endnote file: Endnote
Youth is a key transition period in a person’s life. The health of young people can influence how likely they are to achieve better educational outcomes, make a successful transition into full-time work, develop healthy adult lifestyles, and experience fewer challenges forming families and parenting (AIHW 2021a). A recent survey of youth found that the environment, equity and discrimination, and the economy and financial matters were the top 3 most important issues in Australia today identified by young people (McHale et al. 2023).
This page focuses on key health issues that adolescents and young adults face.
Precise age ranges used for reporting the health of young people varies between data sources, but generally includes teenagers and young adults up to the age of 24. For information about children, see Health of children.
Profile of young people
At 30 June 2023, an estimated 3.3 million young people aged 15–24 lived in Australia. Just over half of these people were male (52%, or 1.7 million) and 48% (1.6 million) were female. Young people aged 15–24 made up 13% of the total population (ABS 2023h).
Australia's young people
In 2022, among all young people aged 15–24:
- Three-quarters (75%) lived in Major cities (AIHW analysis of ABS 2023m)
- One in 5 (20%) lived in the lowest socioeconomic areas (AIHW analysis of ABS 2023m).
- Just over 1 in 5 (21%) were born overseas (ABS 2023b).
As of 30 June 2021, Australian Bureau of Statistics’ (ABS) estimates that 5.3% of young people were Aboriginal and Torres Strait Islander people (ABS 2023a).
Health status of young people
Burden of disease
Burden of disease refers to the quantified impact of a disease or injury on a population, which captures overall health loss, that is, years of healthy life lost through premature death or living with ill health (see Burden of disease).
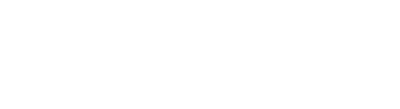
In 2023, mental health conditions, substance use disorders and injuries contributed the most burden for young people aged 15–24. The leading causes of total burden varied between males and females. Suicide and self-inflicted injuries were the leading specific cause of total burden among males, and anxiety disorders were the leading specific cause among females (Figure 1) (AIHW 2023b).
Figure 1: Leading causes of total burden among people aged 15–24, by sex, 2023
This horizontal bar chart shows the top five leading causes of total burden among young people by sex for 2023. The leading cause of burden for females was anxiety disorders (17.1%), followed by: depressive disorders (12%), eating disorders (7.3%), bipolar affective disorder (6.1%), and asthma (5.2%). For males, the leading cause of burden was suicide/self-inflicted injuries (12.7%), followed by: anxiety disorders (10.7%), depressive disorders (6.8%), autism spectrum disorders (5%) and asthma (4.8%).
Chronic conditions
Chronic conditions are an ongoing cause of substantial ill health, disability, and premature death, making them an important global, national and individual health concern. Also referred to as chronic diseases, non-communicable diseases or long-term health conditions, chronic conditions are generally characterised by their long-lasting and persistent effects (AIHW 2023a).
According to self-reported data from the ABS 2022 National Health Survey (NHS), an estimated 3 in 4 (77%) young people aged 15–24 have one or more chronic conditions.
In 2022, the most common chronic conditions among young people aged 15–24 were:
- short sightedness/myopia (28%)
- hay fever and allergic rhinitis (27%)
- anxiety disorders (26%) and depression (17%), both mental and behavioural conditions (ABS 2023c).
Mental health
Measuring mental health
The most recent national data on child and adolescent mental health is from the 2013–14 Australian Child and Adolescent Survey of Mental Health and Wellbeing (also known as the Young Minds Matter survey). Modelling was used to update these estimates. To explore this in more detail, see Regional estimates of child and adolescent mental disorders. However, this report focuses on the original statistics reported at the national level from the Young Minds Matter survey from 2013–14.
Another insight into the mental health and wellbeing of Australians is provided by measures of psychological distress, which may include nervousness, agitation, psychological fatigue and depression. This distress can result in having negative views of the environment, others and oneself, and manifest as symptoms of mental illness, including anxiety and depression (AIHW 2024c).
Surveys which measure psychological distress include the Household, Income and Labour Dynamics in Australia (HILDA) survey, National Study of Mental Health and Wellbeing (NSMHWB) and National Health Survey (NHS).
The ABS recommends that the NSMHWB be used as the main source of prevalence data as it uses diagnostic criteria rather than self-reporting. For more information, see Comparing ABS long-term health conditions data sources.
According to the NSMHWB, in 2020–22, 26% of people aged 16–24 experienced high or very high psychological distress, and young women (34%) were more likely to experience high or very high psychological distress than young men (18%) (ABS 2023i).
Based on self-reported data from the NHS 2022, it was estimated that 20% of people aged 18–24 experienced high or very high levels of psychological distress, and young women were around twice as likely to experience high or very high psychological distress than young men (28% compared with 13%) (ABS 2023f).
In 2013–14, the Young Mind Matters Survey found that around 14% of children aged 12–17 met the clinical criteria for one or more mental disorders in the previous 12 months (Lawrence et al. 2015). The survey also found that anxiety disorders (7.0%) were the most common mental disorder (Table 1). Young males were more likely than young females to have Attention Deficit Hyperactivity Disorder (ADHD) or conduct disorder, while young females were more likely than young males to have anxiety or a major depressive disorder.
For more information, see Mental health.
| Disorder | Males (%) | Females (%) | Persons (%) |
|---|---|---|---|
Anxiety disorders | 6.3 | 7.7 | 7.0 |
ADHD | 9.8 | 2.7 | 6.3 |
Major depressive disorder | 4.3 | 5.8 | 5.0 |
Conduct disorder | 2.6 | 1.6 | 2.1 |
Any mental disorder(a) | 15.9 | 12.8 | 14.4 |
(a) Totals are lower than the sum of disorders as young people may have had more than 1 class of mental disorder in the previous 12 months.
Source: Lawrence et al. 2015.
The Young Minds Matter survey also found that in 2013–14 around 11% of people aged 12–17 had ever deliberately hurt or injured themselves without trying to end their life (self-harmed). Of those young people who had self-harmed, almost three-quarters (73%) had harmed themselves in the previous 12 months. Females aged 16–17 had the highest rates of self-harm, with 17% having harmed themselves in the previous 12 months (Lawrence et al. 2015).
For more information, see Suicide and intentional self-harm.
Disability
Data sources on disability
The Australian Bureau of Statistics’ (ABS) Survey of Disability, Ageing and Carers (SDAC) collects a broad range of information about people with disability including levels of severity, and is the most detailed and comprehensive source of Australian disability data (ABS 2022b).
The 2018 SDAC provides the latest available data and is used on this page to provide information on the prevalence and experiences of disability among young people. Data from the 2022 SDAC is expected to be available from June 2024.
The 2021 Census of Population and Housing collected information on whether a person has a profound or severe core activity limitation, and need assistance in their day to day lives in one or more of the 3 core activity areas of self-care, mobility and communication due to a long-term health condition, a disability or old age. The prevalence of young people with a profound or severe core activity limitations on this page uses self-reported data from the Census.
The prevalence of young people with disability was similar in 2003 and 2018 (9.0% and 9.3%, respectively), with some change in the intervening surveys (6.6% in 2009 and 7.8% in 2012) (ABS 2019a).
Based on self-reported data from the 2018 SDAC, 9.3% of people aged 15–24 had disability (around 291,000 people) (ABS 2019a). The prevalence of disability was similar for males (9.2%) and females (9.5%). Of young people with disability, 6.9% had schooling or employment restrictions (ABS 2019a).
According to the 2021 Census, around 90,000 (3.0%) of people aged 15–24 had severe or profound core activity limitations (ABS 2022a). In comparison, around 66,000 (2.2%) of people aged 15–24 had severe or profound core activity limitations according to the 2016 Census (ABS 2018).
For more information, see Health of people with disability.
Injuries
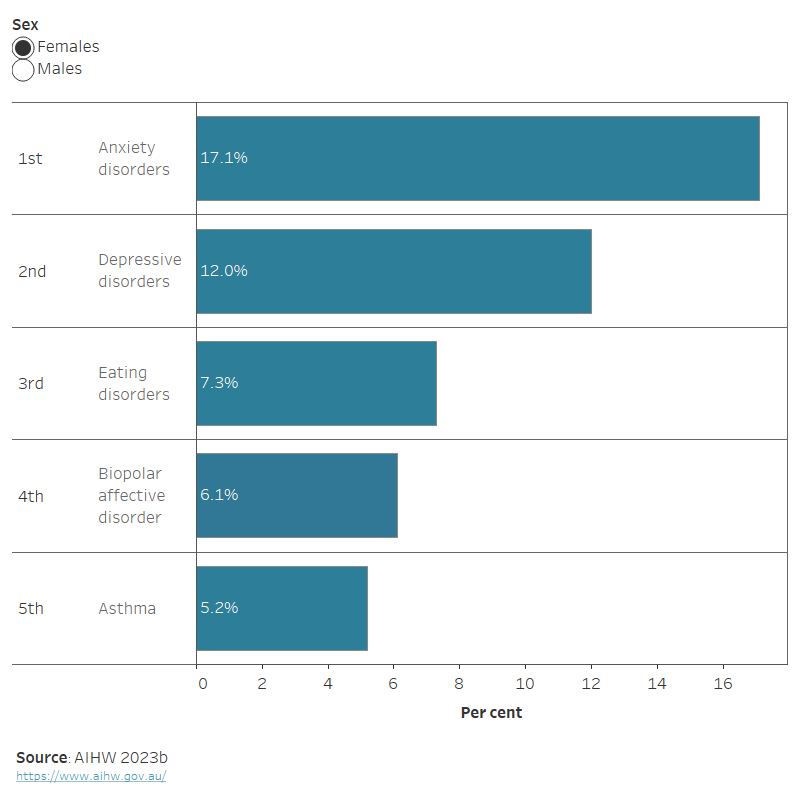
In 2021–22, there were around 68,200 hospitalised injury cases among people aged 15–24 due to injury or poisoning – a rate of 2,200 per 100,000 (AIHW 2023e). The leading causes of injuries for young people were contact with objects (such as being struck or cut by something other than another human or animal), transport accidents and other unintentional causes (if there is no external cause of injury documented in the clinical record, and clarification is unable to be obtained from the clinician) (Figure 2).
For more information, see Injury.
Figure 2: Injury hospitalisations of people aged 15–24, by cause of injury, 2021–22
This horizontal bar chart shows that in 2021–22, contact with objects (18.4%) , transport accidents (17.6%) and other unintentional causes (14.9%) were the 3 leading causes of injury among young people aged 15–24.
Deaths
In 2021, the death rate among people aged 15–24 was 38 deaths per 100,000. The death rate among young people fell between 2009 and 2021, from 41 deaths per 100,000 to 38 deaths per 100,000, respectively. Death rates were higher among young males (52 per 100,000) than females (23 per 100,000) (AIHW 2023d).
Injuries were the leading cause of death among young people, accounting for 809 (69%) of the 1,200 deaths for 15–24-year-olds. Half (50%) of all injury deaths were caused by intentional self-harm (suicide), followed by land transport accidents (28%) and accidental poisoning (8%) (AIHW 2023c, 2023d).
In 2021, young people accounted for 13% of all intentional self-harm deaths. The age-specific rate of intentional self-harm among young people was 13 per 100,000 – an increase from a rate of 9.1 per 100,000 in 2009. The rate of suicide was higher among young males (17.5 per 100,000) than females (8.1 per 100,000) (AIHW 2023d).
For more information, see Life expectancy and causes of death and Suicide and intentional self-harm.
Health risk factors of young people
Overweight and obesity
A healthy body weight is an important factor for a young person’s current and future health, with young people considered overweight or obese more likely to become or remain obese as adults (AIHW 2021b).
Based on measured height and weight data collected through the 2022 NHS, it was estimated that around:
- 1 in 4 (26% or 241,700) 15–17-year-olds were either overweight (18% or 165,400) or obese (9.2% or 84,700).
- 4 in 10 (42% or 909,000) 18–24-year-olds were overweight (27% or 590,300) or obese (14% or 309,200) (ABS 2023e).
For further detail of how overweight and obesity is defined and measured, see Overweight and obesity.
Substance use
Data sources on substance use
A number of nationally representative data sources are available to report on substance use among people aged 14–24. This includes the AIHW National Drug Strategy Household Survey (NDSHS) and the ABS National Health Survey (NHS) for the general population. For more information, see Alcohol, tobacco and other drugs in Australia and the National Drug Strategy Household Survey report 2022–23.
Differences in scope, collection methodology and design may account for variation in estimates reported, and comparisons between collections should be made with caution. For more information, see the technical notes.
In Australia, young people are identified as one of the priority groups in the National Drug Strategy 2017–2026, as they are more vulnerable to behaviours associated with alcohol, tobacco and other drug-related issues which can lead to adverse health and social outcomes (Department of Health 2017).
Tobacco smoking and e-cigarette use
Self-reported data from the 2022–23 NDSHS showed that fewer young people than ever before reported smoking tobacco daily. In 2022–2023, around 10,000 people aged 14–17 and 100,000 people aged 18–24 (compared with 200,000 in 2019) smoked daily in Australia. Consistent with previous years, males aged 18–24 were 1.4 times as likely to smoke daily as females (AIHW 2024d).
In contrast to tobacco, there was a sharp increase in the use of vapes and electronic cigarettes (‘e‑cigarettes’) among young people between 2019 and 2022–23:
- Among people aged 14–17, use of e‑cigarettes increased from 1.8% to 9.7%, becoming the age-group with the third-highest proportion of e‑cigarette use. However, the estimate for 2019 should be interpreted with caution as the relative standard error (see glossary) is between 25% and 50%.
- People aged 18–24 were the most likely to use e‑cigarettes, increasing from 5.3% in 2019 to 21% in 2022–23 (AIHW 2024d).
The NHS 2022 reported on smoking and e-cigarette use among young people aged 15–24. Estimates using self-reported data show that in 2022:
- Among people aged 15–17, 1.6% were daily smokers and 6.8% currently use an e-cigarette/vaping device.
- Nearly 1 in 10 (8.3%) people aged 18–24 were daily smokers and 9.3% currently use an e-cigarette/vaping device (ABS 2023g).
Alcohol consumption
In 2022–23, two-thirds (66%) of people aged 14–17 had never had a full serve of alcohol, compared with 16% of those aged 18–24. Between 2019 and 2022–23, the proportion of 14–17-year-olds consuming 4 or more drinks at least monthly has decreased from 8.9% to 5.5% (AIHW 2024a).
The NHS 2022 reported on alcohol consumption against the 2020 Australian Alcohol Guidelines among 15–24-year-olds. According to self-reported data from the 2022 NHS, around:
- Two in 3 (62%) people aged 15–17 reported they had never consumed a full serve of alcohol.
- One in 7 (14%) people aged 18–24 had never consumed a full serve of alcohol (ABS 2023d).
Use of illicit drugs
Between 2019 and 2022–2023, the proportion of young males who had recently used illicit drugs remained stable. There were however substantial increases in the recent use of illicit drugs among young females, from 9.2% to 17% for those aged 14–17 and from 27% to 35% for those aged 18–24 (AIHW 2024b).
For more information on substance use among young people, see Young people’s use of alcohol, tobacco, e-cigarettes and other drugs.
Sexual and reproductive health
In 2021, the seventh National Survey of Australian Secondary Student and Sexual Health found:
- More than half (61%) of young people aged 14–18 surveyed reported they had sexual experience or were currently sexually active (defined as having experienced oral, vaginal or anal sex).
- Most young people reported that during their most recent sexual experience, they had discussed having sex (80%), sexual pleasure (65%) and using a condom (55%).
- Three-quarters of young people (75%) reported they had a condom available, but only 49% reported using a condom during their most recent sexual encounter.
- Almost three-quarters of young people (72%) agreed that young people should be tested for sexually transmitted infections (STIs). However, young people perceived some barriers with getting tested, with only 39% knowing where they could go to get tested, 26% agreeing that it was easy to get tested, and 33% agreeing that talking to partners about STI testing was difficult.
- A large proportion of students (77%) sought information about sex or sexual health from friends, followed by seeking information from websites (57%) and their mothers (50%), but the most trusted sources of information were general practitioners (GP) (78%).
- Almost all young people (96%) reported that relationship and sexuality education (RSE) is an important part of the school curriculum. Most (93%) reported receiving RSE at school however, only a quarter (25%) reported their most recent RSE class was very or extremely relevant to them (Power et al. 2022).
As the 2021 survey was extensively updated from previous years, comparisons to previous data were not included above. For findings from previous years, see the National Survey of Australian Secondary Students and Sexual Health.
Health care of young people
Mental health services
In 2021–22, people aged 12–24 made up 23% (643,000) of all people receiving Medicare-subsidised mental health-specific services (AIHW 2023f). People aged 18–24 years were most likely to receive services (18% of people aged 18–24 years) and females had a higher rate (13%) compared with males (8%) (AIHW 2023f). Note - an individual may receive a service from more than one type of provider and can be counted more than once.
In 2020–21, the most common provider for people receiving Medicare-subsidised mental health-specific services were General Practitioners (GPs), other psychologists, followed by clinical psychologists. These have remained the same in 2021–22.
For more information, see Mental health services.
Immunisations
The National HPV Vaccination Program has been immunising adolescent girls since 2007 and was extended to boys in 2013. Immunisation against the human papillomavirus (HPV) can prevent cervical and other cancers, and other HPV-related diseases. Since 2023, the routine 2-dose HPV vaccine schedule provided to young people aged 12 to 13 years became a single dose schedule due to changes to the National Immunisation Program (NIP) Schedule.
In 2022, the proportion of 15-year-olds who received at least one dose of the HPV vaccine, compared with 2021, were similar:
- 85% and 86% of girls respectively
- 83% and 84% of boys respectively (NCIRS 2023).
Adolescent HPV vaccination is administered by state and territory health services through school vaccination programs, which also include vaccinations for diphtheria, tetanus and whooping cough (dTpa) and meningococcal disease (types ACWY) (AIHW 2022). In 2022, 87% of young people turning 15 years of age had received their dTpa booster dose and 76% of young people turning 17 years of age had received the meningococcal vaccine (NCIRS 2023).
For more information, see Immunisation and vaccination.
Patient experiences
The ABS Patient Experiences in Australia survey collects information about access and barriers to a range of health care services (ABS 2023k).
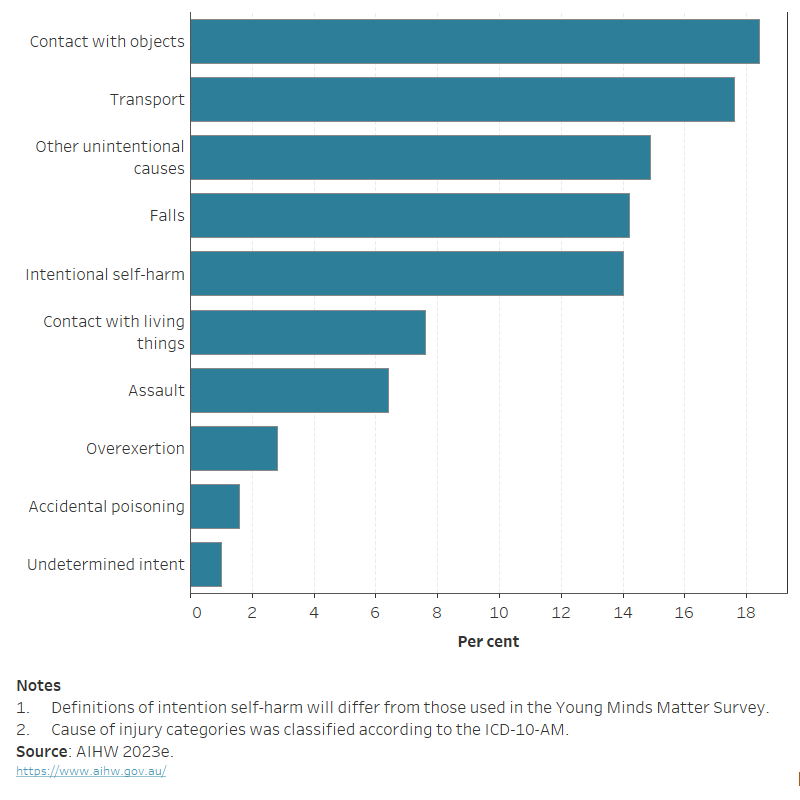
Health service use in 2022–23 remained similar to 2021–22 among 15–24-year-olds who:
- saw an after-hours GP (5.3% compared with 5.2%)
- received a prescription for medication (50.7% compared with 50.1%)
- saw a dental professional (50.8% compared with 49.9%) (ABS 2023i; ABS 2023l).
The proportion of young people who saw a medical specialist or visited hospital emergency department decreased slightly in 2022–23 (ABS 2023l).
In 2022–23, among people aged 15–24, females (27%) were more likely than males (16%) to have used a telehealth appointment for their own health in the last 12 months before the survey. The most common health service used by young people was a GP (Figure 3; ABS 2023l).
Figure 3: Experiences of health services in the last 12 months for people aged 15–24, by sex, 2022–23
This horizontal bar chart shows that in 2022–23, the most common health service used by people aged 15–24 in the 12 months before the survey was: seeing a general practitioner (GP) (70.9%), seeing a dental professional (50.8%), and receiving a prescription for medication (50.7%).
Where do I go for more information?
For more information on the health of young people, see:
- National Youth Information Framework (NYIF) indicators
- Australia's youth
- Aboriginal and Torres Strait Islander adolescent and youth health and wellbeing 2018
- Glossary
For more on this topic, visit Children & youth.
If you or someone you know needs help please call:
Lifeline 13 11 14
Suicide call back service 1300 659 467
Kids Helpline 1800 55 1800
ABS (Australian Bureau of Statistics) (2018) Core Activity Need for Assistance, ABS, Australian Government, accessed 4 March 2024.
ABS (2019a) Disability, Ageing and Carers, Australia: Summary of Findings, ABS, Australian Government, accessed 9 March 2022.
ABS (2022a) Disability and carers: Census - Data table for Disability and carers data summary [data set], abs.gov.au, accessed 17 March 2023.
ABS (2022b) Understanding disability statistics in the Census and the Survey of Disability, Ageing and Carers, ABS website, accessed 27 March 2023.
ABS (2023a) Estimated resident Aboriginal and Torres Strait Islander, non-indigenous and total populations, States and territories – 30 June 2021 [data set], abs.gov.au, accessed 1 March 2024.
ABS (2023b) ‘Estimated resident population, country of birth, age and sex – as at 30 June 1996 to 2022’, ABS Stat Data explorer website, accessed 1 March 2024
ABS (2023c) National Health Survey 2022– Table 3: Long-term health conditions, by age and sex [data set], abs.gov.au, accessed 4 March 2024.
ABS (2023d) National Health Survey 2022- Table 7: Alcohol consumption – Australian Adult Alcohol Guidelines 2020, by age and sex [data set], abs.gov.au, accessed 21 February 2024.
ABS (2023e) National Health Survey 2022 - Table 8: Body Mass Index, waist circumference, height and weight, by age and sex [data set], abs.gov.au, accessed 19 February 2024.
ABS (2023f) National Health Survey 2022 - Table 12: Psychological distress, by age and sex [data set], abs.gov.au, accessed 20 February 2024.
ABS (2023g) National Health Survey 2022 - Table 14: Smoking and vaping, by age and sex [data set], abs.gov.au, accessed 21 February 2024.
ABS (2023h) National, state and territory population – June 2023, ABS website, accessed 9 January 2024.
ABS (2023i) National Study of Mental Health and Wellbeing, ABS website, accessed 20 December 2023.
ABS (2023j) Patient Experiences – 2021–22: Table 1-3 Experience of health services [data set], abs.gov.au, accessed 4 March 2024.
ABS (2023k) Patient Experiences – 2022–23, ABS website, accessed 9 January 2024.
ABS (2023l) Patient Experiences – 2022-23: Table 1-3 Experiences of health services [data set], abs.gov.au, accessed 4 March 2024.
ABS (2023m) Regional population by age and sex [data set], abs.gov.au, accessed 1 March 2024.
AIHW (2021a) Australia's youth, AIHW, Australian Government, accessed 9 March 2022.
AIHW (2021b) Australia’s youth: Body mass index, AIHW, Australian Government, accessed 17 March 2022.
AIHW (2021c) Australia's youth: COVID-19 and the impact on young people, AIHW, Australian Government, accessed 17 February 2022.
AIHW (2022) Immunisation and vaccination, AIHW, Australian Government, accessed 4 March 2024.
AIHW (2023a) Chronic conditions and multimorbidity, AIHW, Australian Government, accessed 4 March 2024.
AIHW (2023b) Data tables: Australian Burden of Disease Study 2023 National estimates for Australia [data set], aihw.gov.au, accessed 9 January 2024.
AIHW (2023c) Deaths in Australia – Data tables: Deaths in Australia [data set], AIHW, Australian Government, accessed 11 July 2023.
AIHW (2023d) General Record of Incidence of Mortality (GRIM) books - Excel workbooks [data set], aihw.gov.au, accessed 11 July 2023.
AIHW (2023e) Injury in Australia – Data tables A: Injury hospitalisations Australia 2021–22 [data set], aihw.gov.au, accessed 6 July 2023.
AIHW (2023f) Medicare-subsidised mental health-specific services – Data tables: Medicare-subsidised mental health-specific services 2021–22 [data set], aihw.gov.au, accessed 14 February 2023.
AIHW (2024a) Data tables: National Drug Strategy Household Survey 2022-23 – 4. Alcohol consumption [data set], aihw.gov.au, accessed 29 February 2024.
AIHW (2024b) Data tables: National Drug Strategy Household Survey 2022–23 – 5. Illicit drugs [data set], aihw.gov.au, accessed 29 February 2024.
AIHW (2024c) Prevalence and impact of mental illness, AIHW, Australian Government, accessed 21 February 2024.
AIHW (2024d) Young people’s use of alcohol, tobacco, e-cigarettes and other drugs, AIHW, Australian Government, accessed 29 February 2024.
Biddle N, Gray M (2022) Tracking wellbeing outcomes during the COVID-19 pandemic (January 2022): Riding the Omicron wave, Centre for Social Research and Methods, Australian National University, accessed 23 May 2022.
Department of Health (2017) National Drug Strategy 2017–2026, Department of Health and Aged Care website, accessed 21 February 2024.
Lawrence D, Johnson S, Hafekost J, Boterhoven De Haan K, Sawyer M, Ainley J and Zubrick SR (2015) The mental health of children and adolescents: report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing, Department of Health, Australian Government, accessed 17 February 2022.
McHale R, Brennan N, Freeburn T, Rossetto A, Richardson E, Boon B and Christie R (2023) Youth Survey Report 2023, Mission Australia, accessed 1 March 2024.
NCIRS (National Centre for Immunisation Research and Surveillance) (2023) Annual Immunisation Coverage Report 2022, NCIRS, accessed 20 December 2023.
Power J, Kauer S, Fisher C, Bellamy R and Bourne A (2022) 7th National survey of secondary students and sexual health 2022, ARCSHS (Australian Research Centre in Sex, Health & Society) monograph series No. 133, La Trobe University website, accessed 9 January 2024.
This page was last updated 16 April 2024. All information on this page is the most recent available, as at that date.