Prescription medications
Definition of PBS prescription medications
The Australian Government subsidises the cost of a wide range of prescription medicines through two separate schemes, the Pharmaceutical Benefits Scheme (PBS) and the Repatriation Pharmaceutical Benefits Scheme (RPBS). Claims for reimbursement for the supply of PBS- or RPBS-subsidised medicines are submitted by pharmacies through Services Australia for processing, and are provided to the Australian Government Department of Health. Subsidies for prescription medicines are available to all Australian residents who hold a current Medicare card, and overseas visitors from countries with which Australia has a Reciprocal Health Care Agreement. In general, patients pay a contribution to the cost of the medicine (co-payment), and the Australian Government covers the remaining cost. This remaining cost is referred to as the benefit paid.
PBS data in this report are from records of prescriptions dispensed under the two schemes, where either:
- the Australian Government paid a subsidy
- the prescription was dispensed at a price less than the relevant patient co-payment (under co-payment prescriptions) and did not attract a subsidy
- PBS data cover all PBS prescriptions dispensed by approved suppliers, including community pharmacies, public and private hospital pharmacies and dispensing doctors.
PBS does not cover:
- over-the-counter purchases
- private prescriptions
- medicines supplied to admitted patients in public hospitals, although prescriptions to patients on discharge and non-admitted patients in all states and territories are in scope, except for New South Wales and the Australian Capital Territory.
The percentage of patients accessing prescription medications rose from 30% of the cohort in the month before initial TBI hospitalisation to 43% of patients in the month after hospitalisation (Figure 23; Table S17). Across the two years before and after hospitalisation, the percentage of the cohort accessing prescriptions medications rose from 24% 24 months before initial TBI hospitalisation to 32% in the 24 months after.
Figure 23: Number of cohort patients with prescriptions dispensed before and after initial TBI hospitalisation
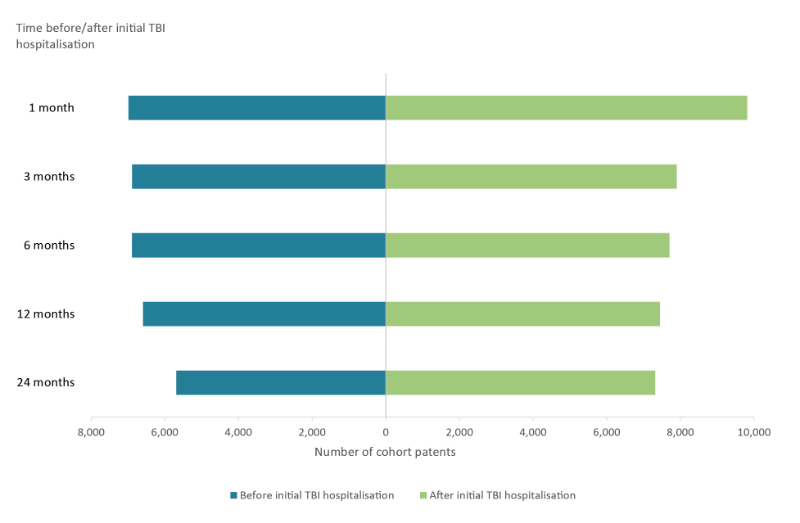
Note: Prescriptions in the 1 month following index admission exclude prescriptions dispensed during admission.
Source: AIHW NIHSI AA v0.5.
Looking more closely at the 2-month mark before and after the initial TBI hospitalisation, the number of different prescription medications dispensed to cohort patients 2 months before hospitalisation compared to 2 months after the initial TBI hospitalisation rose (Figure 24; Table S18).
Figure 24: Number of different prescription medications dispensed to cohort patients 2 months before and after initial TBI hospitalisation
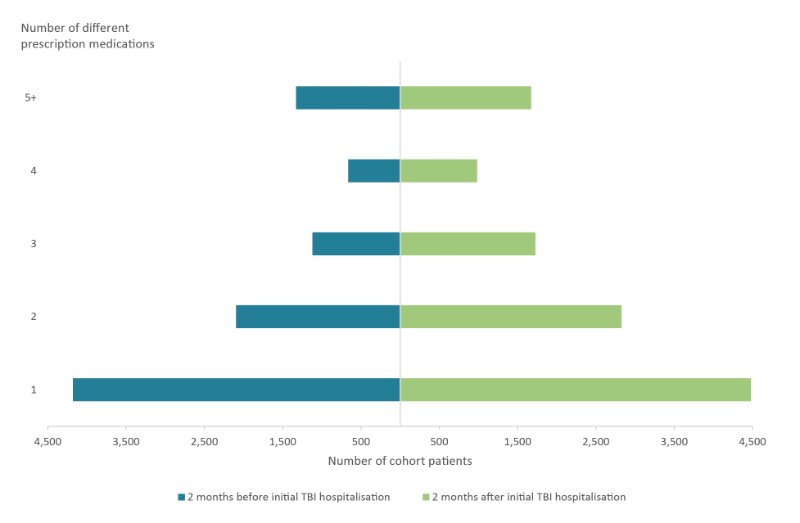
Source: AIHW NIHSI AA v0.5.
The number of different types of prescription medications being dispensed at these two time points is shown in Figure 25, with analgesics for pain relief, antibacterials (antibiotics) and psychoanaleptics (antidepressants) the most commonly prescribed medications (see also Table S19). However, the medications with the largest increase in number of patients receiving them were analgesics (143% increase between the two points in time), anti-epileptics (73% increase) and anti-thrombotics, used to prevent embolisms (58% increase).
Figure 25: Type of prescription medications dispensed 2 months before and after initial TBI hospitalisation
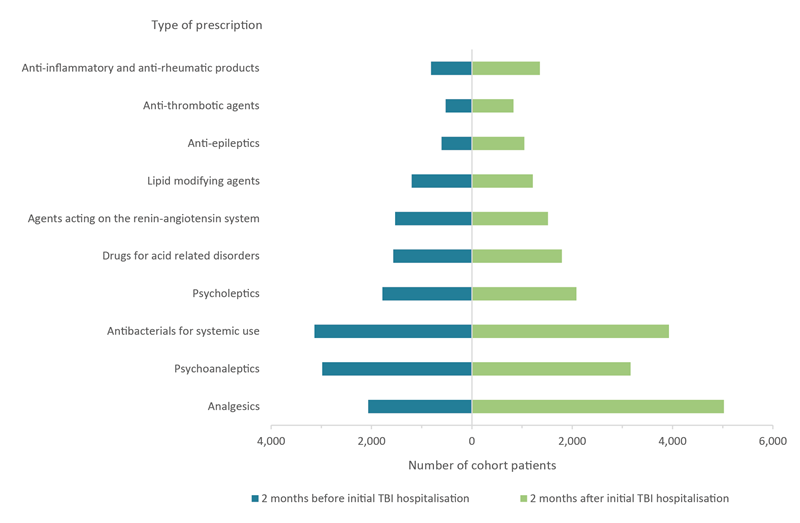
Source: AIHW NIHSI AA v0.5.


