Condition severity
The following measures may indicate the severity of patients’ conditions: length of stay in hospital and whether the patient needed intensive care and/or continuous ventilatory support. In addition to a TBI diagnosis, many patients had other non-TBI related diagnoses and the data presented here indicate the patients’ condition to all diagnoses, not only the TBI diagnoses.
Length of stay in hospital
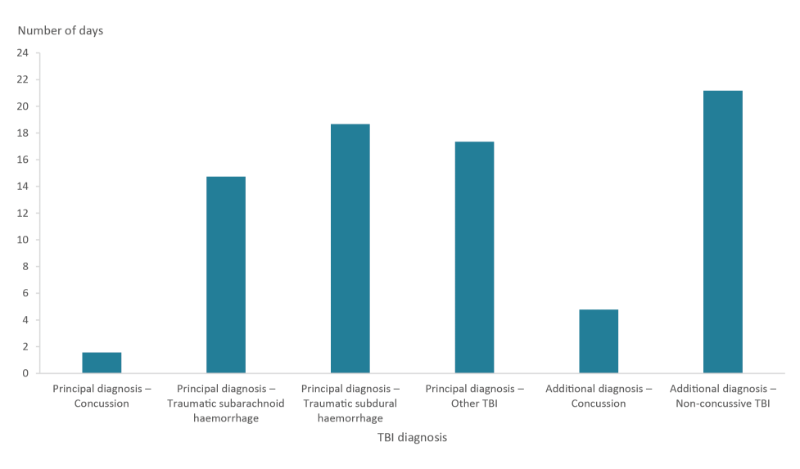
The average number of days patients in the cohort stayed in hospital for an initial TBI was 6.8 days. The average length of stay varied by type of TBI diagnosis (Figure 12; Table S5), with concussive injuries requiring the shortest stays in hospital.
Figure 12: Average number of days cohort patients were hospitalised for initial TBI by TBI diagnosis
Continuous ventilator support
One measure that may indicate the severity of a hospitalised injury is the need for continuous ventilator support (CVS).
Definition of continuous ventilator support
“CVS or invasive ventilation refers to the application of ventilation via an invasive artificial airway […] provided via an endotracheal tube (ETT) or a tracheostomy tube. With CVS, the patient receives continuous variable degrees of assistance to meet respiratory requirements in an uninterrupted continuous fashion.”
– ACHI Coding standard 1006 (ACHI 8th edition)
Overall, 8.3% of patients in the cohort received CVS, reflecting the large number of concussion TBIs, which were much less likely to require CVS than other patients with other types of TBI. Only 2.6% of concussion TBI cases (where TBI was the principal or an additional diagnosis) received CVS (Table 3; Table S6). Among cases with a type of TBI other than concussion (as either a principal or an additional TBI), 24% of patients received CVS.
| Type of TBI diagnosis | Number of patients with CVS | % of patients with CVS |
|---|---|---|
| Principal diagnosis – Concussion | 148 | 1.5 |
| Principal diagnosis – Traumatic subarachnoid haemorrhage | 296 | 25.9 |
| Principal diagnosis – Traumatic subdural haemorrhage | 366 | 25.5 |
| Principal diagnosis – Other TBI | 486 | 24.6 |
| Additional diagnosis – Concussion | 299 | 4.1 |
| Additional diagnosis – Non-concussive TBI | 350 | 21.4 |
| Total | 1,941 | 8.3 |
Source: AIHW NIHSI AA v0.5.
Intensive care
Another measure that may indicate the severity of a hospitalised injury is the percentage of cases involving time in an intensive care unit (ICU). Eleven per cent of patients in the cohort spent time in an ICU, but there was a marked difference according to type of TBI diagnosis. Only 4.2% of concussion TBI cases (where TBI was the principal or additional diagnosis) spent time in an intensive care unit (Table 4; Table S6). Among cases with a type of TBI (as either a principal or an additional TBI) other than concussion, 31% of patients spent time in an ICU.
| Type of TBI diagnosis | Number of patients with time in ICU | % of patients with time in ICU |
|---|---|---|
| Principal diagnosis – Concussion | 188 | 1.9 |
| Principal diagnosis – Traumatic subarachnoid haemorrhage | 355 | 31.1 |
| Principal diagnosis – Traumatic subdural haemorrhage | 471 | 32.8 |
| Principal diagnosis – Other TBI | 562 | 28.5 |
| Additional diagnosis – Concussion | 529 | 7.3 |
| Additional diagnosis – Non-concussive TBI | 500 | 30.6 |
| Total | 2,605 | 11.1 |
Source: AIHW NIHSI AA v0.5.


