 Birthweight
Birthweight
Birthweight is the first weight of the baby obtained after birth. Birthweight is reported in 3 categories: low birthweight (birthweight less than 2,500 grams), healthy birthweight (birthweight between 2,500 and 4,499 grams) and high birthweight (birthweight of 4,500 grams or more).
Babies with birthweights outside the healthy range are at greater risk of illness, poor development, perinatal death, and poorer health in adulthood. Babies with a low birthweight are more likely to experience illness or die in infancy, have poorer development of their mental functioning abilities, and have an increased risk of chronic diseases in adulthood (AIHW 2022a).
A high birthweight is associated with an increased risk of adverse maternal outcomes such as emergency caesarean section and postpartum haemorrhage, impairment and injury of the newborn, and hypertension, obesity, and type 2 diabetes in later life (AIHW 2022a).
According to a recent report, factors related to the mother that contribute to low birthweight for Aboriginal and Torres Strait Islander babies are maternal smoking, the mother being underweight pre-pregnancy, and the mother not having access to antenatal care in the first trimester (AIHW 2022b). Additional factors associated with low birthweight are maternal health conditions such as pre-existing and gestational hypertension and pre-existing diabetes (AIHW 2022b).
The National Agreement on Closing the Gap (the National Agreement) includes a target to increase the proportion of Aboriginal and Torres Strait Islander babies with a healthy birthweight to 91% by 2031 (Productivity Commission 2020). It is important to note that indicators under this target influence birthweight, and progress to increase healthy birthweight will influence all other targets under the National Agreement.
Aboriginal and Torres Strait Islander babies are more likely to have a healthy birthweight when they are born to mothers who have access to culturally safe antenatal care – early and regularly throughout their pregnancy – intrapartum care and postnatal care (AIHW 2022b; HCA 2019).
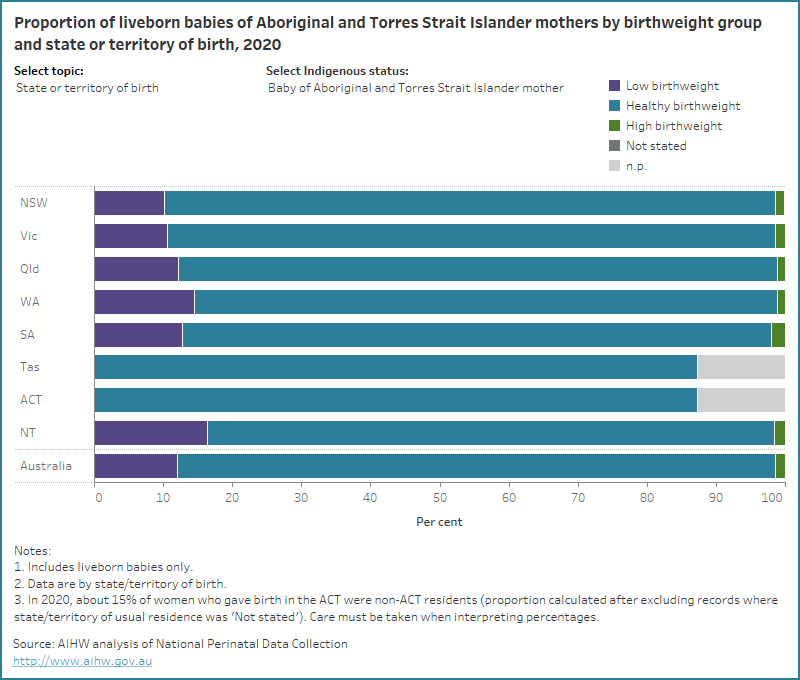
In 2020, 12% of liveborn babies of Aboriginal and Torres Strait Islander mothers were of low birthweight, 87% had a healthy birthweight and 1.4% were of high birthweight (compared with 6.2%, 93% and 1.2%, respectively, of babies of non-Indigenous mothers).
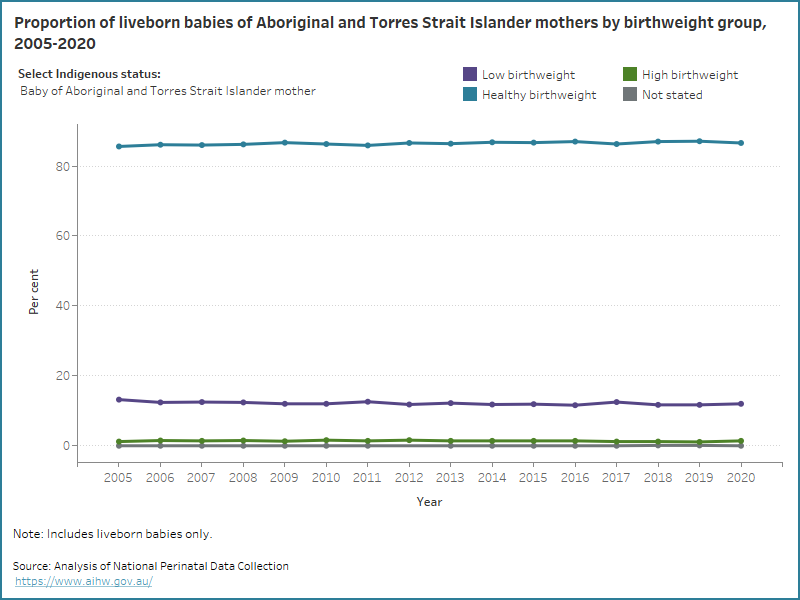
Over time, the proportion of babies of Aboriginal and Torres Strait Islander mothers by birthweight group has remained largely unchanged. Between 2005 and 2020, the proportion of those of low birthweight ranged from 12% to 13%, those born with a healthy birthweight ranged from 86% to 87% and those born with a high birthweight ranged from 1.1% to 1.6%.
The data visualisation below shows the proportion of liveborn babies of Aboriginal and Torres Strait Islander mothers and non-Indigenous mothers by birthweight group from 2005, and the proportion of liveborn Aboriginal and Torres Strait Islander babies and non-Indigenous babies by birthweight group from 2013.
Figure 1: Proportion of babies of Aboriginal and Torres Strait Islander mothers, babies of non-Indigenous mothers, Aboriginal and Torres Strait Islander babies and non-Indigenous babies, by birthweight group from 2005 to 2020
Line graph of birthweight group by Indigenous status. Most liveborn babies of Aboriginal and Torres Strait Islander mothers had a healthy birthweight.
In 2020, liveborn babies who were born to Aboriginal and Torres Strait Islander mothers were more likely to have a healthy birthweight if they were born:
- at term (94%, compared with 37% of pre-term babies)
- to mothers who lived in the least disadvantaged areas (90%, compared with 86% for the most disadvantaged areas)
- to mothers who lived in Inner regional areas or Major cities (both 88%, compared with 83% for Remote or Very remote areas)
- to mothers aged 20-24 years or 25-29 years (both 87%, compared with 84% for those born to mothers aged under 20 years)
- to mothers with a parity of 1 (88%, compared with 84% of those whose mother had a parity of 4 or more)
- to mothers who did not smoke (90%, compared with 82% of those whose mother smoked).
The data visualisation below presents data on birthweight group for liveborn babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies, by selected maternal and baby characteristics for 2020.
Figure 2: Proportion of liveborn babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies by birthweight group and selected topic for 2020
Bar chart for birthweight group by selected topics. 87% of liveborn babies of Aboriginal and Torres Strait Islander had a healthy birthweight
Being born with a healthy birthweight was more common in some geographical locations. Explore the map below to view data on the number and proportion of liveborn babies of Aboriginal and Torres Strait Islander mothers and liveborn Aboriginal and Torres Strait Islander babies who were born with a healthy birthweight, by IREG and PHN for 2020 and SA3 for 2017-2020.
Figure 3: Proportion of liveborn babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies with a healthy birthweight by various geographies
Map of proportions of liveborn babies of Aboriginal and Torres Strait Islander mothers and liveborn Aboriginal and Torres Strait Islander babies who were born with a healthy birthweight across Australia grouped by various geographies.
For related information see:
- the Regional Insights for Indigenous Communities section on Birthweight.
- Aboriginal and Torres Strait Islander Health Performance Framework indicator 1.01 Birthweight.
References
AIHW (Australian Institute of Health and Welfare) (2022a) 1.01 Birthweight, Aboriginal and Torres Strait Islander Health Performance Framework website, accessed 17 October, 2022.
AIHW (2022b) Aboriginal and Torres Strait Islander Health Performance Framework: Key factors contributing to low birthweight among Aboriginal and Torres Strait Islander babies, Cat. no. IHPF 10 Canberra: AIHW.
HCA (Murawin Consulting and Human Capital Alliance) (2019) Final Report of the 2016-18 Evaluation of the AMIHS program. Sydney: NSW Ministry of Health.
Productivity Commission (2020) National Agreement on Closing the Gap [website], accessed 20 March, 2023.


