 Analgesia
Analgesia
Pain during labour and birth is affected by physiological and psychological factors, and the effectiveness of pain relief administered during labour is affected by maternal expectations of – and anxiety related to – pain (Schug et al. 2015). Choice of pain relief (whether pharmacological or non-pharmacological) is influenced by maternal health conditions, experiences during previous pregnancies, the health professionals involved in providing maternity care, and the setting of birth (Steel et al. 2015).
As analgesia is used to relieve pain during labour, data are limited to mothers who had labour, whether spontaneous or induced (note that some mothers who labour may go on to have a caesarean section and receive anaesthesia rather than analgesia). More than one type of analgesic can be administered.
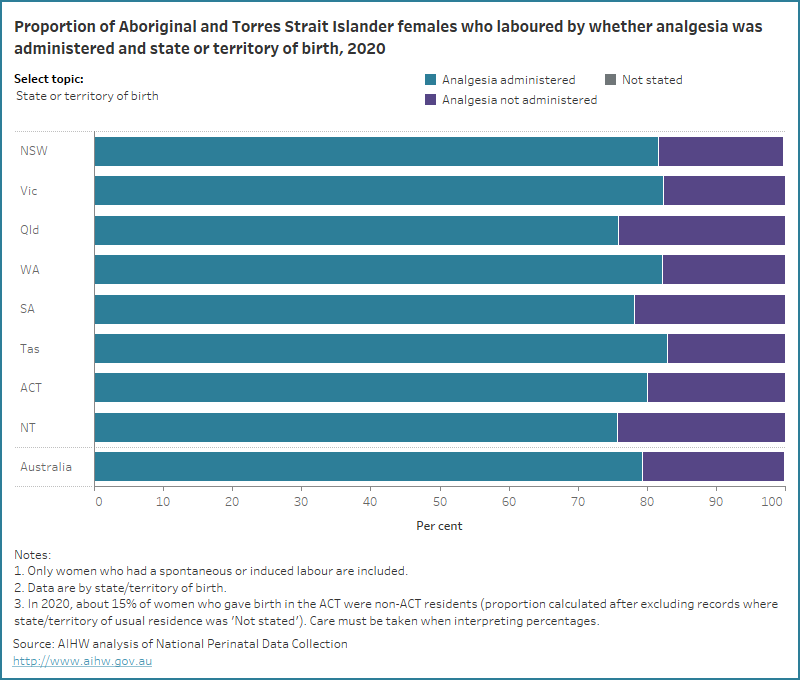
In 2020, 79% of Aboriginal and Torres Strait Islander females who gave birth and laboured had analgesia administered (which was the same as for non-Indigenous females). The proportion of Aboriginal and Torres Strait Islander mothers who laboured and had analgesia has increased over time (from 72% in 2010 to 77% in 2020).
Nitrous oxide was the most common type of analgesia used (61 per 100 Aboriginal and Torres Strait Islander females who laboured), followed by epidural or caudal analgesia (29 per 100) and systemic opioids (17 per 100) (compared with 52 per 100 non- Aboriginal and Torres Strait Islander females who laboured for nitrous oxide, 41 per 100 for epidural or caudal analgesia and 12 per 100 for systemic opioids).
The data visualisation below shows the proportion of Aboriginal and Torres Strait Islander and non-Indigenous females who laboured by analgesia administration status, from 2010.
Figure 1: Proportion of Aboriginal and Torres Strait Islander females and non-Indigenous females who gave birth by analgesia administration status from 2010 to 2020
Line graph of analgesia administration status and Indigenous status. Aboriginal and Torres Strait Islander mothers receiving analgesia increased.

In 2020, greater proportions of Aboriginal and Torres Strait Islander females who gave birth were administered analgesia if they:
- lived in Major cities (81%, compared with 73% of Very remote areas)
- were aged under 20 years (87%, compared with 71% of those aged 35-39 years)
- were first-time mothers (90%, compared with 67% of those with a parity of 4 or more)
- had induced labour (88%, compared with 73% for spontaneous labour)
- had an instrumental vaginal birth (94%, compared with 77% of non-instrumental vaginal births).
The data visualisation below presents data on analgesia administration status for Aboriginal and Torres Strait Islander females who laboured, by selected maternal characteristics for 2020.
Figure 2: Proportion of Aboriginal and Torres Strait Islander females who laboured by whether analgesia was administered and selected topic for 2020
Bar chart for analgesia administration status by selected topics. 80% of Aboriginal and Torres Strait Islander mothers received analgesia.
References
Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J (2015) Acute Pain Management: Scientific Evidence (4th edition) Melbourne: Acute Pain Management Scientific Evidence Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine.
Steel A, Adams J, Sibbritt D, Broom A, Gallois C and Frawley J (2015). ‘Managing the pain of labour: factors associated with the use of labour pain management for pregnant Australian women’, Health Expectations 18(5), doi:10.1111/hex.12155


