Maternal and perinatal mortality
Maternal mortality
Between 2006 and 2020, 186,777 Aboriginal and Torres Strait Islander females gave birth and there were 28 maternal deaths for Aboriginal and Torres Strait Islander females, with a maternal mortality ratio of 16.9 per 100, 000 Aboriginal and Torres Strait Islander females giving birth (maternal mortality ratio calculation excludes WA between 2006 and 2017).
Box 1: Defining maternal death
Maternal death is the death of a woman while pregnant or within 42 days of the end of pregnancy, irrespective of the duration and outcome of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
Of these maternal deaths, 16 were direct maternal deaths (resulting from obstetric complications of pregnancy or its management) and 12 were indirect maternal deaths (resulting from diseases or conditions that were not due to a direct obstetric cause but were aggravated by the physiologic effects of pregnancy).
Sepsis and thromboembolism were the most common causes of death for direct deaths (both 3) and cardiovascular conditions were the most common cause of death for indirect deaths (6).
Between 2006 to 2020, there were also 10 coincidental maternal deaths (deaths during pregnancy or the postpartum period that were unrelated to pregnancy) for Aboriginal and Torres Strait Islander females for example, due to motor vehicle trauma.
Table 1 shows the number of direct and indirect maternal deaths of Aboriginal and Torres Strait Islander females, by cause, pregnancy status and selected characteristics.
| Direct deaths | Indirect deaths | Total deaths | |
|---|---|---|---|
| Cause of death | |||
| Cardiovascular | 1 | 6 | 7 |
| Non-obstetric haemorrhage | 0 | 1 | 1 |
| Suicide | 1 | 1 | 2 |
| Sepsis | 3 | 3 | 6 |
| Thromboembolism | 3 | 0 | 3 |
| Obstetric haemorrhage | 2 | 0 | 2 |
| Amniotic fluid embolism | 1 | 0 | 1 |
| Hypertensive disorders | 2 | 0 | 2 |
| Respiratory failure(b) | 0 | 1 | 1 |
| Substance use complications | 1 | 0 | 1 |
| Anaesthetic-related death(c) | 2 | 0 | 2 |
| Total | 16 | 12 | 28 |
| Timing of death(d) | |||
| Antepartum | 2 | 6 | 8 |
| Day of birth (day 0) | 2 | 0 | 2 |
| Postpartum | 7 | 2 | 9 |
| Not stated/supplied | 3 | 3 | 6 |
| Total | 14 | 11 | 25 |
| Maternal age at death | |||
| Under 20 | 1 | 3 | 4 |
| 20-24 | 3 | 0 | 3 |
| 25-29 | 3 | 3 | 6 |
| 30-34 | 3 | 2 | 5 |
| 35-39 | 2 | 1 | 3 |
| 40 or over | 1 | 0 | 1 |
| Not stated/supplied | 3 | 3 | 6 |
| Total | 16 | 12 | 28 |
| Parity(e) | |||
| None | 2 | 4 | 6 |
| One | 1 | 0 | 1 |
| Two | 3 | 3 | 6 |
| Three | 1 | 0 | 1 |
| Four or more | 5 | 1 | 6 |
| Not stated/supplied | 4 | 4 | 8 |
| Total | 16 | 12 | 28 |
a) Data on Indigenous status are not available for WA for 2006-2017.
b) Respiratory failure due to Asthma complicated by Pneumonia.
c) Anaesthetic-related deaths were not classified separately prior to 2012.
d) Data excludes maternal deaths where pregnancy status at time of death was ‘termination of pregnancy’ or ‘miscarried’.
e) Parity refers to a woman’s number of previous pregnancies resulting in live births or stillbirths, excluding the current pregnancy.
Perinatal mortality
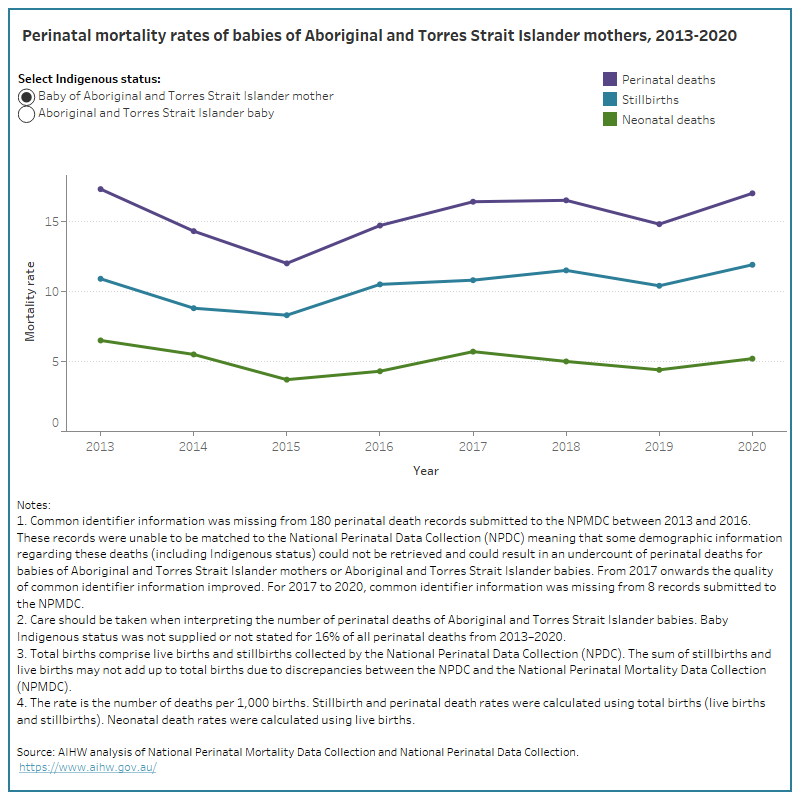
In 2020, there were 14,605 babies born to Aboriginal and Torres Strait Islander mothers and 249 perinatal deaths, with a perinatal mortality rate of 17 deaths per 1,000 births. Of these perinatal deaths, 174 (70%) were stillbirths and 75 (30%) were neonatal deaths, with a stillbirth rate of 12 deaths per 1,000 births and a neonatal mortality rate of 5.2 deaths per 1,000 live births.
Between 2013 and 2020, there were 109,308 babies born to Aboriginal and Torres Strait Islander mothers and 1,682 perinatal deaths; 1,140 (68%) of these were stillbirths and 542 (32%) were neonatal deaths.
During this period, the perinatal mortality rate for babies of Aboriginal and Torres Strait Islander mothers fluctuated between 12 and 17 deaths per 1,000 births, as did the stillbirth and neonatal mortality rate (between 8.3 and 12 deaths per 1,000 births and between 3.7 and 6.5 deaths per 1,000 live births, respectively).
The data visualisation below presents data on perinatal mortality rates, stillbirth rates and neonatal mortality rates for babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies from 2013 to 2020.
Figure 1: Perinatal mortality rates of babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies from 2013 to 2020
Line graph shows that perinatal mortality rates for babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies have fluctuated over time.
Timing of death
Between 2013 and 2020, there were 1,438 perinatal deaths of babies of Aboriginal and Torres Strait Islander mothers where the timing of perinatal death was recorded. Of these:
- 50% (735) occurred as stillbirths prior to birth (antepartum period)
- 14% (208) occurred as stillbirths during the labour or birth (intrapartum period)
- 24% (355) were very early neonatal deaths (within the first 24 hours following birth)
- 6.5% (97) were early neonatal deaths (1-7 days following birth)
- 5.9% (88) were late neonatal deaths (8-28 days following birth).
The data visualisation below presents data on the timing of perinatal deaths, stillbirths and neonatal deaths for babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies for 2013 to 2020 combined.
Figure 2: Proportion of babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies who died by timing of death for 2013 to 2020
Bar chart showing the timing of perinatal death. 50% of perinatal deaths were antepartum stillbirths.
Cause of death
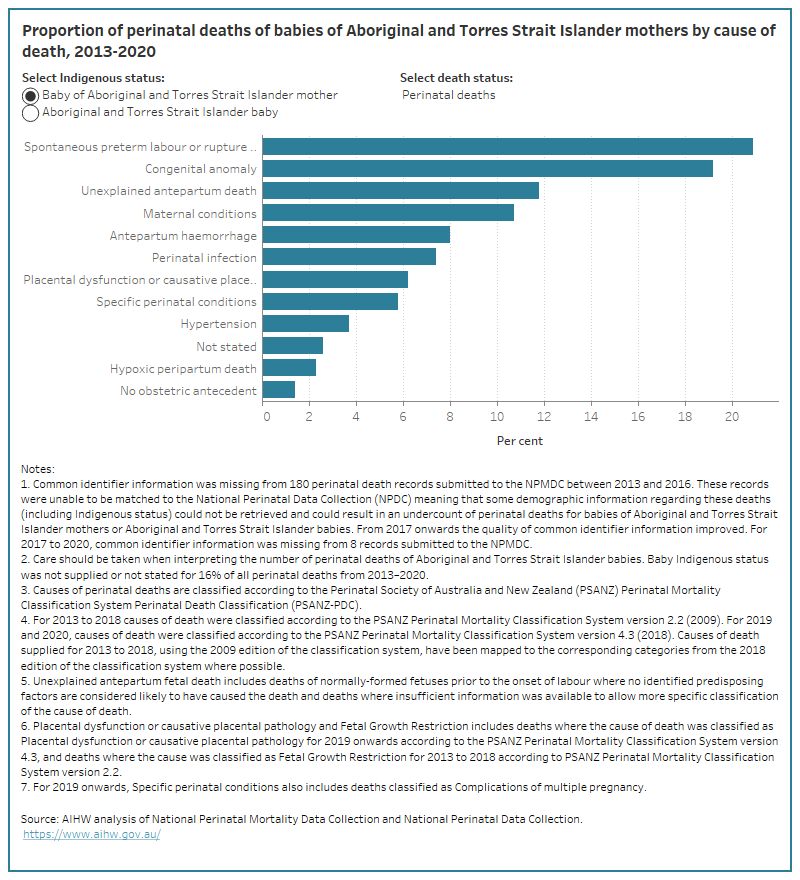
Between 2013 and 2020, the 3 most common causes of perinatal death (classified according to the Perinatal Society of Australia and New Zealand (PSANZ) Perinatal Mortality Classification System) were spontaneous pre-term labour or rupture of membranes (<37 weeks gestation) (21% (352)), congenital anomaly (19% (323)) and unexplained antepartum death (12% (199)).
The most common causes of:
- stillbirths were congenital anomaly (18% (201)), unexplained antepartum death (18% (199)) and maternal conditions (14% (161))
- neonatal deaths were spontaneous pre-term labour or rupture of membranes (<37 weeks gestation) (38% (208)), congenital anomaly (23% (122)) and perinatal infection (7.7% (42)).
The data visualisation below presents data on the causes of perinatal deaths, stillbirths and neonatal deaths for babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies for 2013 to 2020 combined.
Figure 3: Proportion of perinatal deaths of babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies by cause of death and selected death status for 2013 to 2020
Bar chart showing the cause of perinatal death. Spontaneous preterm labour or rupture of membranes was the most common cause of perinatal death.
Maternal and baby characteristics
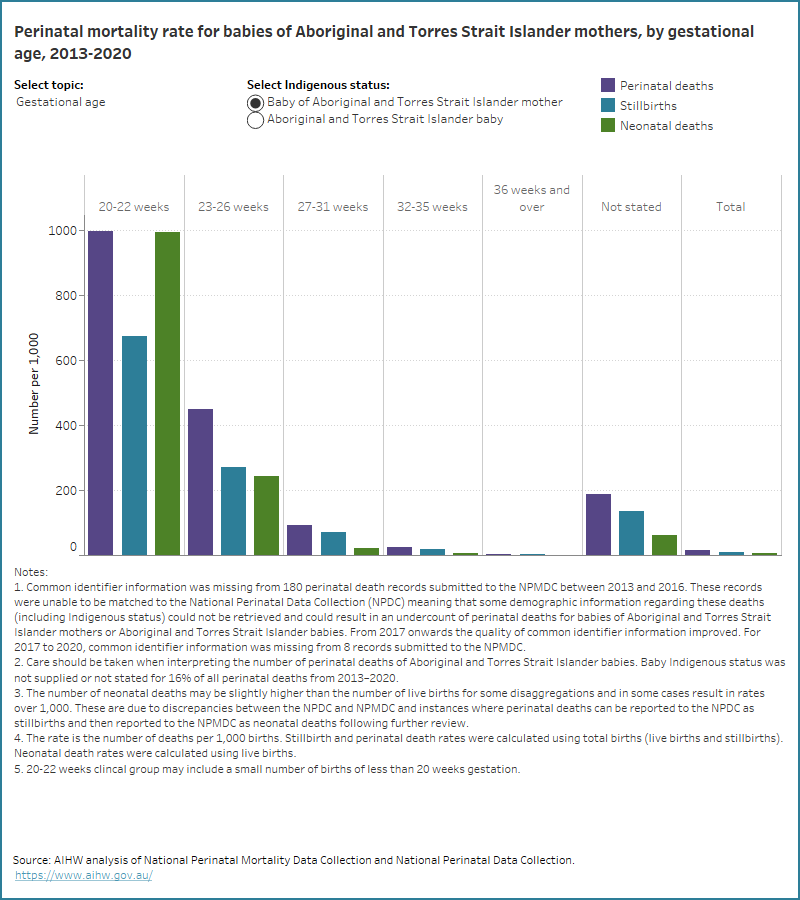
Between 2013 and 2020, the perinatal mortality rate was higher for certain groups of babies born to Aboriginal and Torres Strait Islander mothers, including babies:
- of low birthweight (100 per 1,000 births, compared with 2.8 per 1,000 healthy birthweight babies)
- babies who had a gestational age of 20-22 weeks (997 per 1,000 births, compared with 3.3 per 1,000 of babies with a gestational age of 36 weeks and over)
- whose mothers had pre-existing diabetes (41 per 1,000 births, compared with 20 per 1,000 with a diabetes status of none or not stated and 6.4 per 1,000 with gestational diabetes)
- whose mothers were aged 40 years and over (26 per 1,000 births, compared with 13 per 1,000 whose mothers were aged 25-29 years)
- whose mothers were underweight (24 per 1,000 births) or obese (20 per 1,000) (compared with 18 per 1,000 whose mothers were normal weight or overweight)
- whose mothers lived in Very remote areas (23 per 1,000 births, compared with 13 per 1,000 babies whose mothers lived in Inner regional areas or Major cities).
Similarly, the stillbirth rate was higher for babies of Aboriginal and Torres Strait Islander mothers who were:
- of low birthweight (67 per 1,000 births, compared with 1.9 per 1,000 healthy birthweight babies)
- 20-22 weeks gestational age (676 per 1,000 births, compared with 2.2 per 1,000 babies with a gestational age of 36 weeks and over)
- born to mothers who had pre-existing diabetes (32 per 1,000 births, compared with 13 per 1,000 with a diabetes status of none or not stated and 4.2 per 1,000 with gestational diabetes)
- born to mothers aged 40 years and over (18 per 1,000 births, compared with 8.7 per 1,000 whose mothers were aged 25-29 years)
- born to mothers who lived in Very remote areas (14 per 1,000 births, compared with 8.8 per 1,000 babies whose mothers lived in Inner regional areas).
The neonatal mortality rate was highest for babies of Aboriginal and Torres Strait Islander mothers who were:
- of low birthweight (35 per 1,000 livebirths, compared with 0.9 per 1,000 healthy birthweight babies)
- 20-22 weeks gestational age (995 per 1,000 livebirths, compared with 1.1 per 1,000 babies with a gestational age of 36 weeks and over)
- born to mothers were underweight (10 per 1,000 livebirths, compared with 5.8 per 1,000 whose mothers were normal weight)
- born to mothers who lived in Very remote areas (8.9 per 1,000 livebirths, compared with 3.7 per 1,000 babies whose mothers lived in Major cities)
- born to mothers who had pre-existing diabetes (8.6 per 1,000 livebirths, compared with 6.6 per 1,000 with a diabetes status of none or not stated and 2.3 per 1,000 with gestational diabetes).
It is important to note that whilst the characteristics listed above are more commonly found in women with pregnancies resulting in stillbirth and neonatal death, it is not implied that they are the cause of perinatal deaths.
The data visualisation below presents data on perinatal deaths, stillbirths and neonatal deaths for selected maternal and baby characteristics, for babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies, for 2013 to 2020 combined.
Figure 4: Perinatal mortality rate for babies of Aboriginal and Torres Strait Islander mothers and Aboriginal and Torres Strait Islander babies by selected topic for 2013 to 2020
Bar chart showing the rates of perinatal deaths by selected topics. The highest rates of perinatal death occurred at 20-22 weeks gestation.