Health services used by people with younger onset dementia
Services provided by health professionals, including primary health care providers (such as general practitioners, or GPs), other medical specialists (such as geriatricians and psychiatrists) and allied health professionals (such as physiotherapists and speech pathologists), as well as prescribed medications, play a crucial role in the diagnosis, treatment and/or management of dementia.
The following sections present statistics and information on:
For more information on health service use by people with dementia of all ages, see Health services used by people with dementia.
Primary health care services used by people with younger onset dementia
The following section presents data that are currently available on the use of primary health care services by people with dementia through services provided under the Medicare Benefits Scheme (MBS).
Dementia diagnostic information is not available in the MBS, so it is not possible to distinguish between dementia-specific services and services for the management of other health issues. These data are sourced from linked health and aged care services data in the National Health Data Hub (AIHW NHDH 2020–21), previously referred to as the National Integration Health Services Information (NIHSI) analytical asset. Identification of people with dementia depends on their use of other health and aged care services (for example, through admission to hospital or entry to permanent residential aged care), so the information below will not include all younger people with dementia in Australia.
Results of this analysis should be interpreted with caution due to data limitations. For more information on data considerations of this analysis, refer to the Technical notes.
In 2020–21, there were nearly 11,700 people aged 30–64 who were identified as having dementia in the linked data (Table S7.2). Of these, just over 2,000 (17%) lived in permanent residential aged care for all or part of the year (this is a higher proportion than the estimate in the prevalence section because people in the later stages of dementia are more likely to be identified in the linked data than people in the early to moderate stages).
Among people with younger onset dementia (aged 30–64), those living in the community used an average of 36 MBS services and those living in permanent residential aged care used an average of 46 MBS services (Table S7.2). This was similar for those aged 65 years and older, with an average of 38 MBS services used by those living in the community and an average of 45 MBS services used by those in permanent residential aged care.
- Percentage of people who used a service: ‘Percentage’ is the proportion of people with at least one service recorded in the linked data in 2020–21. This is also referred to as a rate of service use.
- Average number of services per person: The average number of services per person was calculated for people who used the service at least once in 2020–21, referred to in figure as ‘Mean (service user)’.
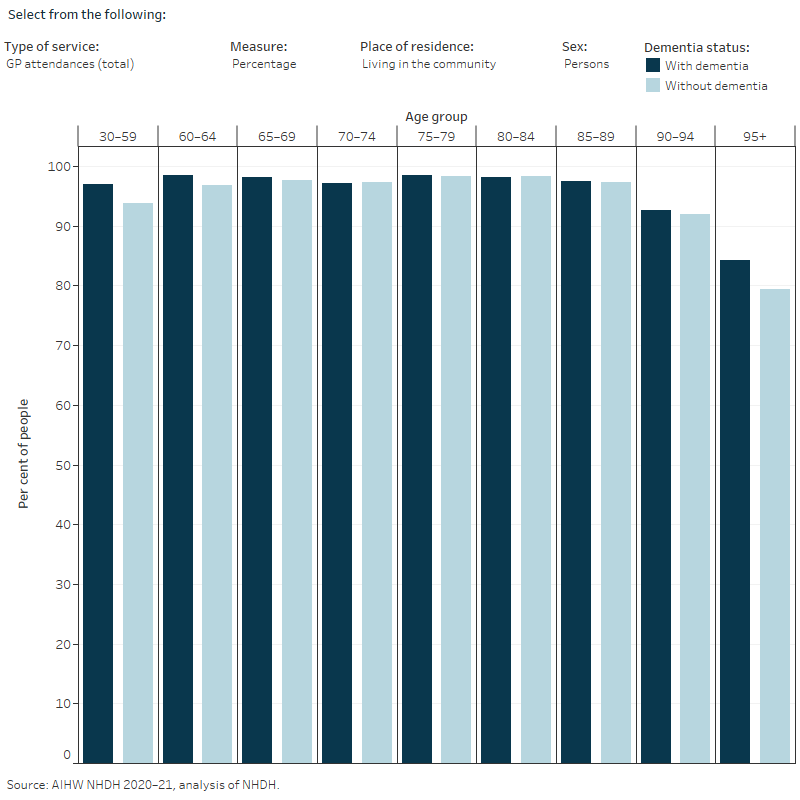
These measures reflect different aspects of access to services. For example, for people living in the community, more people living with dementia had one or more GP chronic disease management attendances than those without dementia in the age groups 30–80 years. However, among people who used the service, there was little difference in the average number of attendances.
Health service attendances for people living in the community
Among people aged 30–59, living in the community and who had used a particular MBS service at least once, the average number of attendances for certain services was greater for people with dementia than for those without dementia, and this difference tended to decrease in the older age groups (Figure 7.2). The MBS services where people aged 30–59 with dementia had a greater number of attendances than those without dementia were:
- GP attendances (17 attendances for people with dementia compared to 7.3 for those without dementia).
- Specialist attendances (4.8 for people with dementia compared to 3.0 for those without dementia). This difference was largely driven by differences in the number of geriatric medicine, neurology, and general medicine attendances.
- Allied health attendances (3.4 for people with dementia compared to 2.5 for those without dementia). Within allied health attendances, podiatry and optometry followed a similar pattern.
- Pathology services (14 for people with dementia compared to 9.1 for those without dementia).
- Diagnostic imaging (3.4 for people with dementia compared to 2.7 for those without dementia).
- Nurse attendances (2.4 nurse attendances per person), this was higher than those without dementia (1.8) of the same age, and all other age groups with or without dementia.
Figure 7.2: MBS service use by type of service, place of residence, sex and age
Bar graph showing that younger people with dementia had a greater average number of attendances for certain services compared to those without dementia, such as GP services for those living in the community, and psychiatry attendances for those living in PRAC.
Health service attendances while living in permanent residential aged care
In 2020–21, people with dementia aged 30–59 years living in permanent residential aged care had a greater average number of nurse attendances per person (6.0) than those without dementia of the same age (4.6). This age group had the largest difference in average nurse attendances between those with or without dementia, although older age groups tended to follow this pattern as well.
Those aged 30–59 with dementia had the highest average number of general medicine attendances per person (4.0) compared to those of the same age without dementia (1.8), and all other age-groups. Aside from people aged 95 years or older, people aged 30–59 were the only age group to have a greater average number of psychiatry attendances per person (4.4) than those without dementia (3.8).
For more information on MBS services used by people with dementia see Primary health care services.
Medications dispensed to people with younger onset dementia
While there is currently no known cure for dementia, there are four medications available under the Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Benefits Scheme (RPBS) that may assist in managing dementia symptoms and slow dementia progression. In Australia, these medications are currently only subsidised for people with a diagnosis of Alzheimer’s disease. This section focuses on dispensing patterns of dementia-specific medications supplied to people aged 30–64, under the PBS and RPBS.
It is important to note that information on medication intake and adherence to medication plans is not available. The data presented here relate only to prescriptions dispensed. In addition, the PBS and RPBS do not contain data on dispensing of privately prescribed medications (prescriptions that are not eligible for subsidy under the PBS or RPBS), medications to public hospital in-patients and over-the-counter medications. For more information on dementia-specific medications see Prescriptions for dementia-specific medications.
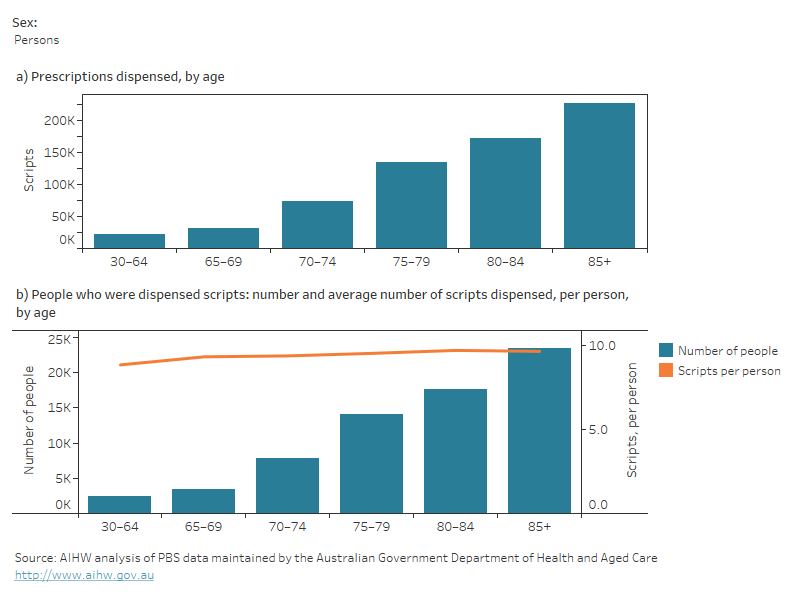
Prescriptions for dementia-specific medications varied with age
In 2021–22, nearly 2,500 people aged 30–64 were dispensed nearly 21,800 dementia-specific medications (Figure 8.1a). The average number of scripts dispensed per person was lower for people aged 30–64 (8.9 per person) than for people aged 85 and over (9.7 per person) (Figure 8.1b).
Figure 8.1: Dementia-specific medications by age and sex in 2021–22: (a) numbers of prescriptions dispensed and (b) number of people who were dispensed scripts and average number of scripts dispensed per person
Two graphs on prescriptions dispensed for dementia-specific medications to people aged 30 and over by age and sex in 2021-22. The first is a bar graph showing the number of scripts dispensed by age group. The second is a bar and line graph, with the bar graph showing the number of people who were dispensed scripts for dementia-specific medications and the line graph showing the average number of scripts dispensed per person, both broken down by age groups. The number of prescriptions dispensed, the number of people dispensed scripts and the average number of scripts dispensed per person all increased with age. A greater number of women were dispensed a greater number of scripts than men.
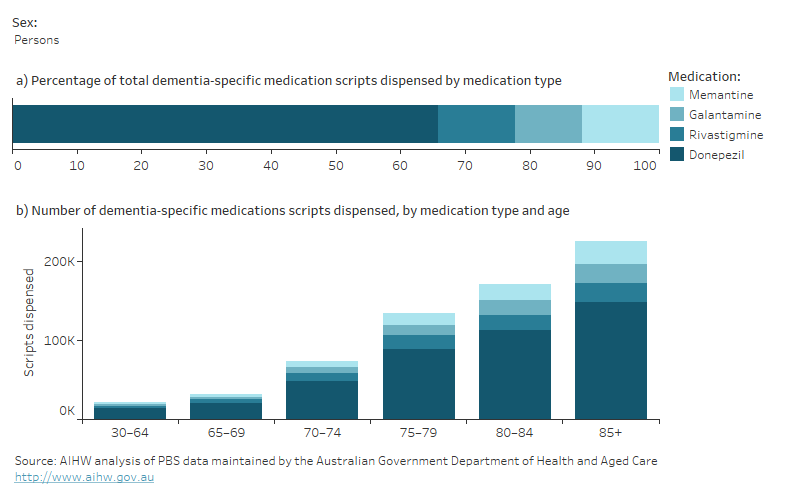
Donepezil was the most dispensed dementia-specific medication in 2021–22 for people aged 30–64, accounting for about 14,000 prescriptions or 64% of all dementia-specific scripts dispensed (Figure 8.3). Memantine, usually prescribed for moderately severe to severe Alzheimer’s disease, accounted for 14.2%.
Figure 8.3: Dementia-specific medications, by medication type and sex in 2021–22: (a) percentage of all scripts dispensed by medication type and (b) number of scripts dispensed by medication type and age
Two graphs on the prescriptions dispensed for dementia-specific medications, by the four types of dementia-specific medications and sex in 2021-22. The first graph is a stacked bar graph showing the percentage of all scripts dispensed by medication type. The second graph is a stacked bar graph showing the number of scripts dispensed by medication type and age. Around two-thirds of prescriptions dispensed for dementia-specific medications were for Donepezil, and this was the most commonly dispensed medication in each age group in both men and women. Women were dispensed a greater number of scripts than men for each of dementia-specific medication.
In 2021–22, the proportion of people who were dispensed scripts for dementia-specific medications for the first time varied by age: 1 in 3 people (34%) aged 30–64 were dispensed scripts for the first time (Table S8.5). This decreased to almost 1 in 5 people (18%) among those aged 85 and over.
As people with dementia often have other co-existing conditions, they are likely to be prescribed a range of other medications. For people who were dispensed scripts for dementia-specific medications in 2021–22, psychoanaleptics (medications used to treat depression and other neurological and mental disorders) were dispensed to a larger proportion of people aged 30–64 (61%) compared with people aged 85 and over (48%) (Table S8.8). However, most other medications were dispensed to a greater proportion of people aged 85 and over.
People with younger onset dementia were more likely to be dispensed antipsychotic medications
People with dementia may experience changed behaviours, such as aggression, agitation and delusions, commonly known as behavioural and psychological symptoms of dementia (BPSD). To manage these symptoms, non-pharmacological interventions are recommended, but medical professionals may prescribe antipsychotic medications to people with dementia with BPSD as a last resort.
In 2021–22, among people dispensed scripts for dementia-specific medication, people aged 30–64 were more likely to also be dispensed antipsychotic medications (which are part of the psycholeptics group): 23% of women and 25% of men aged 30–64, compared with 20% of men and 19% of women aged 85 and over (Table S8.9).
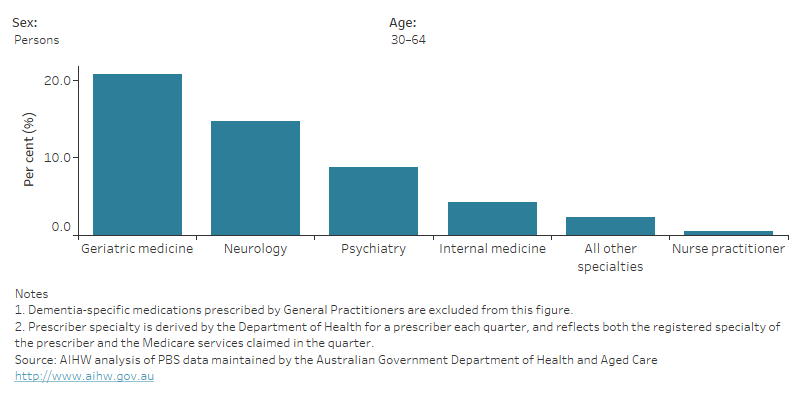
Prescribers of dementia-specific medications to people with younger onset dementia
In 2021–22, 3 in 4 people (74%) aged 30–64 who were dispensed scripts for dementia-specific medications were prescribed at least one script by a general practitioner (GP), compared with 84% of people aged 65 and over (Table S8.15).
As younger people aged 30–64 are less likely to see a doctor with a specialisation in geriatric medicine, a greater proportion of dementia-specific medications were prescribed by neurologists (15%) and psychiatrists (8.7%) than they were for people aged 65 and over (4.2% and 3.5%, respectively) (see Figure 8.9).
Figure 8.9: People who were dispensed dementia-specific medications in 2021–22: percentage by medical speciality of prescriber, age and sex
Bar graph showing that younger people were more likely to be prescribed dementia-specific medicines by neurologists and psychiatrists than people aged 65 years or more.
Hospitalisations of people with younger onset dementia
This section includes information on the number and characteristics of dementia-related episodes of admitted patient care (referred to as 'hospitalisations') from the National Hospital Morbidity Database, including hospitalisations due to dementia in 2021–22. Hospitalisations due to dementia refer to hospitalisations where dementia was the main reason for the admission to hospital. For more information see Hospital care.
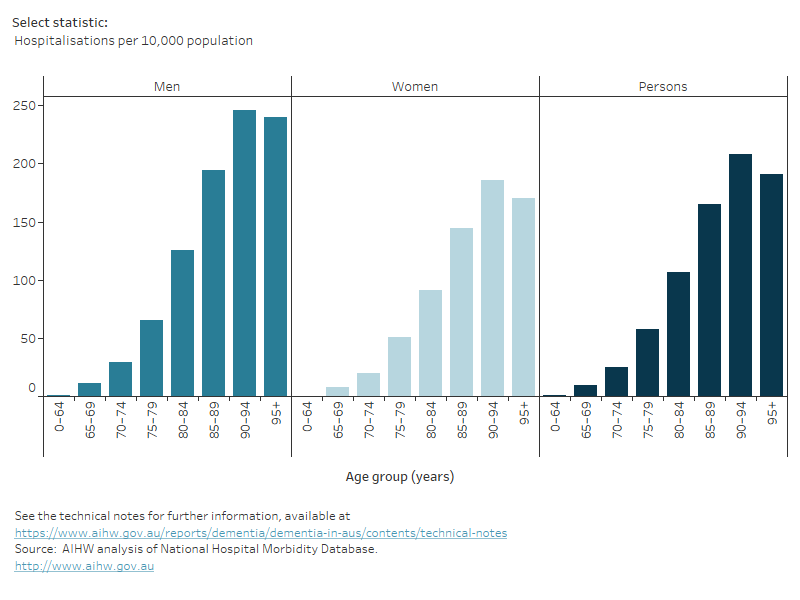
With increasing age, hospitalisations due to dementia increased in number but decreased in length
In 2021–22, people aged 0–64 had the lowest number of hospitalisations due to dementia (just over 1,000) compared to all other age groups except those aged 95 and over (995 hospitalisations). While having fewer hospitalisations, people aged 0–64 had the longest average length of stay in hospital (31 days) than all other age groups, decreasing to an average of 11 days among people aged 95 and over (see Figure 9.1).
Figure 9.1: Overview of hospitalisation due to dementia in 2021–22, by age and sex
Bar graph showing that younger people with dementia tend to have fewer hospitalisations but a longer average length of stay in hospital than older people with dementia.
AIHW (2020–21) National Health Data System, aihw.gov.au, accessed 10 February 2024.
Draper B and Withall A (2016) ‘Young onset dementia’, Intern Med J, 46(7):779-786, doi:10.1111/imj.13099.


