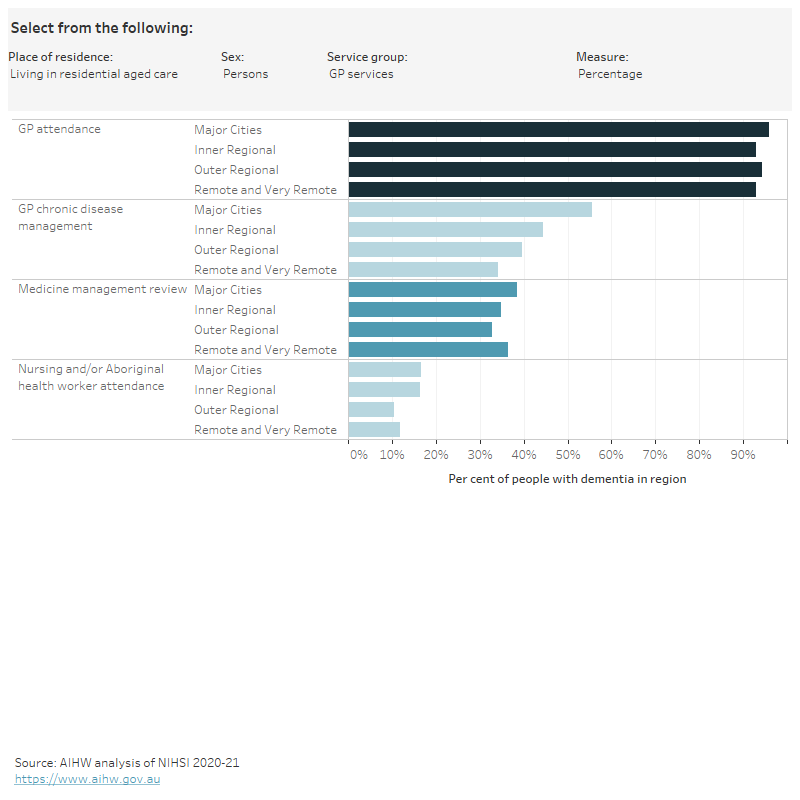
Rates of health service use by remoteness area
Figure 2.2 is an interactive chart exploring the use of health services by remoteness area, with rates (the percentage of people in the dementia study cohort with at least one service), rate ratios (where rates for people living in Major cities were used as a reference point to compare with other remoteness areas) and age-standardised rates.
People living in the community
People living with dementia in the community in Remote and very remote areas of Australia had lower rates of:
- specialist attendances
- dispensing of dementia-specific medications
- emergency department visits
- allied health attendances – podiatry
but higher rates of:
- medication management review attendances
- hospital stays
than people living in Major cities.
The dispensing of opioids tended to be higher in regional and remote areas, especially for women. People living in regional and remote areas also had higher rates of nursing and/or Aboriginal health worker attendances.
There was a similar rate of service use across remoteness areas for GP attendances and the dispensing of antipsychotics, benzodiazepines and glucose regulating medications.
People living in Inner regional areas tended to have similar rates of health service use as people in Major cities, with the exception of lower rates of specialist attendances and the dispensing of dementia-specific medications.
Rates were highest in Inner regional areas and decreased with increasing remoteness for:
- GP chronic disease management attendances
- allied health attendances – total and optometry
- polypharmacy and the dispensing of antidepressants.
People living in residential aged care
There was a similar rate of service use across remoteness areas for GP attendances and the dispensing of antidepressants and antipsychotics.
People living with dementia in residential aged care in Inner regional, Outer regional and Remote and very remote areas of Australia had lower rates of:
- specialist attendances
- GP chronic disease management attendances
- nursing and/or Aboriginal health worker attendances
- allied health attendances
- polypharmacy and hyper-polypharmacy
- medication management review attendances
- dispensing of dementia-specific medication
- dispensing of benzodiazepines
- emergency department visits
- hospital stays (although Outer regional rates were similar to Major cities)
than people living in Major cities.
People living in Remote and very remote areas also had lower rates of dispensing of cardiovascular and glucose regulating medications, whereas rates for these services in Inner and outer regional areas were similar to Major cities.
Rates of opioid dispensing were highest in Inner regional areas and decreased with increasing remoteness.
People living with dementia who had a GP chronic disease management (CDM) plan were more likely to have a Medicare-subsidised allied health care attendance than people without a CDM plan, at all remoteness areas. For example, among people living in the community in Inner regional areas, 81% of those with a CDM plan in 2019 also had an allied health attendance, compared with 42% of those without a CDM plan (Table S2.13).
Figure 2.2: Health service use among people in the dementia cohort, by place of residence, remoteness area and sex, 2019
Figure 2.2 is an interactive bar chart showing variation in the use of a range of health services by remoteness area for people in the dementia study cohort living in the community or living in residential aged care. Health services groups shown are GP services, specialist services, allied health services, ED visits, hospital stays, polypharmacy and medications dispensed (1 or more, 4 or more). Measures of use are percentage of people who used the service, age-standardised rates and rate ratios.
Notes
- The dementia study cohort refers to 158,730 people aged 30 and over who were living in Australia in 2019 and had a dementia record in the NIHSI. Western Australia and the Northern Territory were excluded from all analyses because their hospital data were not available for construction of the cohort.
- The geographies in this report are based on where a person lived, not where they received services. Remoteness areas are based on the 2016 Remoteness Area Structure within the ASGS.
- ‘Percentage’ is the proportion of people in the dementia cohort with at least one service recorded in the NIHSI in 2019.
- Rate ratios are a method for comparing rates between regions. The rates for people living with dementia in Major cities were used as the reference population to compare with other remoteness areas. A rate ratio of 1 indicates that the rate for the region is the same as the rate in the reference population. A rate ratio greater than 1 indicates that the rate for the region is higher than the rate in the reference population. A rate ratio less than 1 indicates that the rate for the region is lower than the rate in the reference population.
- Age-standardised rates were calculated where population and service counts allowed.
- Only public hospital data were included in this analysis: some of the observed variation may be due to the availability and use of private hospitals.
- The bar is blank if a value could not be published due to data quality or confidentiality concerns.
Data tables: Health service use among people in the dementia cohort