Full-time equivalent staffing
People in custody often require more medical attention than the general population.
People in prison are more likely than those of the same age in the community to have mental health disorders or chronic physical health conditions, and are less likely to have sought, or have had access to, clinical health services in the community (Young et al. 2015).
For many, prison provides the opportunity to see health professionals, and to receive the treatment they require. When healthier people are released from prison, the entire community benefits (Kinner and Young 2018).
The provision of health-care services to people in prison depends on the availability of suitably qualified staff. People in custody should have access to health care that is equivalent to that in the community, taking into consideration the need for health-care professionals that specialise in mental health, and in alcohol and other drug use disorders. Medical and allied health services should be provided onsite, wherever possible (Australian Medical Association 2012; United Nations 1990).
The number of health-care staff required in a prison depends on factors such as:
- whether the prison is a reception centre where complete medical examinations are performed
- whether the prison is a females’s prison, as medical requirements for males and females differ
- requirements for drug and alcohol detoxification.
Staffing discussed in this report is restricted to doctors and nurses, for which there is more consistent reporting across jurisdictions.
In 2021, there were 3.81 full-time equivalent doctors and nurses working within the correctional system per 100 people in custody (Indicator 3.1.15).
In 2021, there were 0.39 full-time equivalent (FTE) doctors and 3.42 FTE nurses practising in prison clinics per 100 people in custody (from a total of 35,722 people in custody on 30 June 2021 in participating facilities and jurisdictions) (Figure 10.12).
In the 2022 collection, jurisdictions were asked to provide a standard FTE of doctors and nurses in all prison clinics for the 2021 calendar year. So, any comparisons with previous versions of this data collection should not be made.
The FTE rate of doctors and nurses in prison clinics (3.81 FTE per 100) was over twice that of the equivalent rate in the general population (1.61 FTE per 100) (Figure 10.12).
For doctors, the rate in prison clinics (0.39 FTE per 100 persons) was similar to that in the general community in Australia (0.42 FTE per 100 persons). But the rate of nurses in prison clinics (3.42 FTE per 100 persons) was more than 2.5 times that in the general Australian population in 2020 (1.19 FTE per 100 persons) (AIHW 2022).
This likely reflects the greater need for health-care services in prisons, and the nurse-led primary health-care model provided in prison clinics, along with medication administration models that differ from those in the community due to the secure prison environment.
Figure 10.12: FTE health professionals in Australian prisons (2021) and in Australia (2020) (rate)
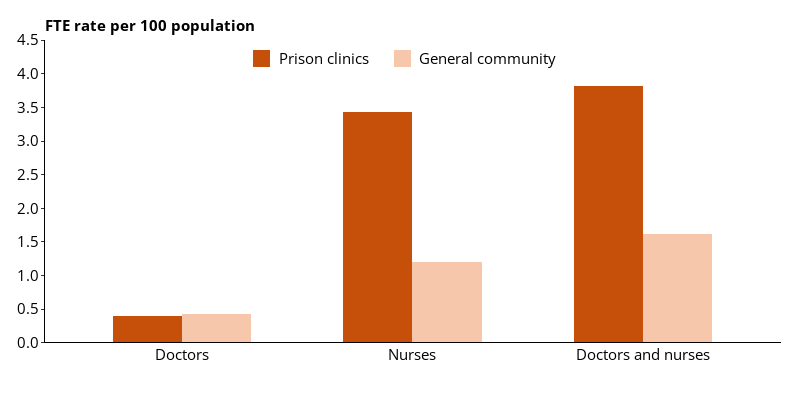
Note: Excludes Victoria, which did not provide data for this item.
Sources: 2022 NPHDC; AIHW 2022.
AIHW (Australian Institute of Health and Welfare) (2022) Health workforce, AIHW website, accessed 1 June 2023.
Australian Medical Association 2012 Position statement on health and criminal justice system, Australian Medical Association, Canberra.
Kinner SA and Young JT (2018) ‘Understanding and improving the health of people who experience incarceration: an overview and synthesis’, Epidemiologic Reviews, 40(1):4–11, doi:10.1093/epirev/mxx018.
United Nations (1990) Basic principles for the treatment of prisoners, [universal instrument], adopted 14 December 1990 by General Assembly resolution 45/111.
Young JT, Arnold-Reed D, Preen D, Bulsara M, Lennox N and Kinner SA (2015) ‘Early primary care physician contact and health service utilisation in a large sample of recently released ex-prisoners in Australia: prospective cohort study’, BMJ Open, 5:e008021, doi:10.1136/bmjopen–2015–008021.


